latest update 01/14/2025 (work in progress) Notes from lectures from doctors at Memorial Sloan Kettering Cancer Center’s Fundamentals of Oncology Acupuncture.
Integrative Medicine core Lecture Series.
| Oncology | |
| Understanding Cancer | |
| The nature of Cancer Cells | Uncontrollable growth |
| Spreading to other parts of body | |
| One cell has a genetic mutation | |
| Hyperplasia- few few cells grow | |
| Dysplasia- mass forms | |
| in situ cancer- tumor (in place, not spread) | |
| Invasive Cancer- to blood vessel/lymph and spread | |
| Causes | Genetics |
| Exposure to harmful elements | |
| lack of protective elements | |
| Chance | |
| Cell Cycle | Cell grows- decides whether to continue, replication of DNA- |
| Cell prepares to divide- cell division (mitosis). | |
| a break in this cycle “check and balance” cause cancer. | |
| DNA-RNA-Protein-> function. Gene mutation cause malfunction | |
| DNA and protein | Dna is the blueprint |
| Protein is the building blocks. | |
| Gene mutations | Missense mutation- Dna code for an amino acid- replacement of a single nucleotide- |
| Incorrect amino acid which may produce a malfunctioning protein. | |
| Nonsense mutation- same as above but causing a shortening of the protein. | |
| One small change creates a whole function change in the cell. | |
| Chromosomes | Normal is 23 pairs, but an abnormal set might have missing, 3, or extra genes. |
| Mutations | Most of the time, cancer cells harbor multiple mutations. First, second, third, fourth. |
| fourth or later mutations become malignant cell. | |
| Similar, like kid having bad influences like friends, books, movies. Change gradually over time. | |
| APC mutation | |
| Try to stop early -> | cox-2 over expression (non-dysplastic ACF) anti inflammatory may prevent cancer. |
| K-ras mutation (Dysplastic ACF low grade) | |
| p53 mutation (Dysplastic ACF high grade) | |
| Loss of 18q (Adenocarcinoma) years to develop | |
| Traditional hallmarks of Cancer | Sustaining proliferative signaling (grow) |
| Evading growth suppressors (ignore cell death and keep growing) | |
| Activating invasion and metastasis (cells that travel on and move) | |
| enabling replicative immortality (cells that don’t die off when job is finished) | |
| Inducing angiogenesis (cells that attract blood vessels to grow the cancer with nutrients) | |
| Resisting cell death (resist immune cells) | |
| Inducing angiogenesis (cells that attract blood vessels to grow the cancer with nutrients) | |
| Cells of Tumor microenvironment | CSC- cancer stem cell (mother cells) |
| CAF- Cancer Associated Fibroblast | |
| EC- Endothelial Cell | |
| PC- Pericyte | |
| CC- Cancer cell | |
| Ics- Immune inflammatory cell | |
| Emerging hallmarks in Cancer | Avoiding immune destruction- Cancer cells have fake ID that they are good. |
| Tumor-promoting inflammation- reduce inflammation | |
| Genome instability and mutation- genes, proof readers broken | |
| Deregulating cellular energetics (how cancer use sugars, glucose, to grow) starve the cancer. | |
| Cancer diagnosis | Symptoms |
| Physical examination | |
| Blood tests (cancer markers and proteins that suggest cancer) PSA for example prostate. | |
| X-ray and Scans | |
| Biopsy (Gold standard) cells under microscope. Can show how aggressive. | |
| Biopsy : molecular markers. Ex.- estrogen receptors. Positive with particular dye. | |
| Type of cancer confirmed by biopsy. Tissue type is more important than anatomical location. | |
| Where it came from is more important than where it is. | |
| Men most common Cancer | Prostate 27%, Lung 14%, Colon 8%, UB 7% |
| Women most common cancer | Breast 29%, Lung 13%, Colon 8%, Uterine 6% |
| Most common cancer Death: | Lung, Prostate, Breast, Colon, Pancreas, Liver, Ovary, Leukemia |
| Staging | TNM: Tumor Node Metastasis system (Size and amount of lymph nodes involved) |
| Stage 0: in situ. Tis, No, mo | |
| Stage I: T1. no, ,mo | |
| Stage IIa: T0, N1, Mo, or T2, No, Mo | |
| Stage IIb: T2, N1, Mo, orT3, No, Mo | |
| Stage IIIa: t0-2, N2, Mo,or T3, N1-2, Mo | |
| Stage IIIb: T4, N (any), Mo, or T (any) N3, Mo. | |
| Stage IV: T (any), N (any), M1. | |
| Predicts survival rate of 5 years. | |
| Treatment Plan | Surgery- best chance if caught early. Pain, dysfunction, wound, bowel, nutrition def., self-image (mastectomy) |
| Chemo | Chemotherapy- kill or suppress tumor growth. Cell cycle chemo drugs: |
| G0 and G1: p16, PCNA inhibitors, p21, p53, HDM2 modulators, Selicidib (Cyc202), cyc065 | |
| CDk4/D, Xeloda 5-FU, CDK2/E | |
| S: Sapacitabine (CYC682), Gemzar cisplatin, CDk2/A | |
| G2: Camptosar Vepesid | |
| M: Pik1 inhibitors, other mitotic spindle targets, Aurora inhibitors, Taxol, Taxotere | |
| Breast cancer: cyclophoshamide, doxorubicin, paclitaxel | |
| Colon: 5-FU, Oxalipatin, Irinotecan | |
| Lung: cisplatin, docetaxel | |
| Ovarian: Carboplatin, Paclitaxel, Doxorubican | |
| Chemo side effects: Fatigue, nausea, vomiting, poor appetite, constipation, diarrhea, | |
| low blood counts, neuropathy. | |
| Most side effects are mild, but 1/4 is higher, low % is severe. | |
| Targeted therapy | EGFR Inhibitors- attack cancer ability to sustain proliferation signaling |
| Cyclin-dependent kinase inhibitors- attack cancer ability to evade growth suppressors | |
| Immune activating ant CTLA4 mAB-attack cancer ability to avoid immune destruction | |
| Telomerase Inhibitors- attack cancer ability to enable replicative immortality | |
| Selective anti-inflammatory drugs- attack cancer ability to Tumor-promoting inflammation. | |
| Inhibitors of HGF/c-Met- attack cancer ability to activating Invasion and metastasis | |
| PARP inhibitors- attack cancer ability to genome instability and mutation | |
| Proapoptotic BH3 mimetics-attack cancer ability to resisting cell death | |
| Aerobic glycolysis inhibitors- attack cancer ability to deregulate cellular energetics. | |
| Personalized therapy | |
| based on cancer genomics | Treatment tailored to the individual patient based on cancer genomic info |
| Genomic analysis of tumor samples from a individual patient | |
| Identification of “driver alterations” that drive cancer growth and spread | |
| Use of known drugs that attack those alterations as treatment. | |
| Radiation- | Some types of cancer can be cured like lymphoma, but some are resistant |
| Side effects: fatigue, local reaction, fibrosis, secondary cancer | |
| Hormonal therapy | Tamoxifen- block the estrogen receptor |
| side effects: fatigue, postmenopausal symptoms, sexual dysfunctin, wieght gain, joint/mus. Ache | |
| Immunotherapy | Destroy the immunosuppression characteristic of cancer cell so that immune cells can attack. |
| Investigational treatment | to test the safety and efficacy of a new therapy in humans |
| (clinical trials) | clinicaltrials.gov reports 14,889 open studies on cancer as of July 2014 |
| May hold much promise also with unknown side effects. | |
| Cancer survivorship: 5 year rate | 68% all sites since 2003-2009 |
| Prostate is almost 100% in men | |
| Breast is 90% in women. | |
| After treatment: road ahead | Symptoms remain, Recovery (mental/physcial), lifestyle change, prevention, wellness. |
| Integrative medicine has a lot to offer. | |
| summary | Cancer arises form genomic changes in the cancer cells. |
| microenvironment where cancer cells live also plays a important role in how cancer cells behave. | |
| Cancer is not one disease, but hundreds of diseases based on the profile changes in the cells. | |
| Some cancers can be diagnosed early and cured. Once spread most types of cancer are not curable. | |
| Cancer patients have many needs other than just having cancer removed or reduced. | |
| Integrative medicine can address those needs like reduce symptoms, improve quality of life, and | |
| promote a sense of well-being. |
| Cancer Treatment Modalities | |
| Symptom management | |
| Biology of Cancer | Broad group of disease characterized by unregulated cell division and growth |
| Malignant tumors are formed and invade nearby body parts and distal sites. | |
| Causes of cancer are diverse and partially understood. | |
| Cancer Basics | A malignant disease. A series of cellular or genetic changes that cause abnormal cell growth. |
| Tumor formation due to uncontrolled cell growth and invasion of the surrounding tissue. | |
| Ability to spread. Grows and divides quickly. | |
| Treatment modalities | Chemotherapy- systemic treatment, using cytotoxic antineoplastic drugs as standard regimen. |
| Biotherapy- treatment working with patient immune system to fight cancer and control side effects. | |
| Surgery- removal of local tumor | |
| Radiation therapy- external beam and brachytherapy | |
| Chemotherapy works by killing cells that rapidly divide. It does kill normal and malignant cells. | |
| chemo affects cells in the bone marrow, digestive tract and hair follicles. | |
| this can cause myelosupression, mucostits, and alopecia. | |
| chemo toxicites: myelosupression, fatigue, nausea, vomiting, diarrhea, constipation | |
| Anorexia, mucositis, alopecia, “chemo brain”. | |
| Nursing management | Myelosuppression- suppression in bone marrow causing decrease in WBC, RBC, and/or platelets. |
| Nadir: point at which lowest blood cell count is reached. 7-10 days after treatment. | |
| Neutropenia: point at which there is a decrease in neutrophils.**RISK OF INFECTION | |
| ANC determines if treatment can and/or will continue. | |
| Anemia- reduction in hemoglobin or RBC’s in the blood. **3rd/4th cycle of chemo. | |
| thrombocytopenia: lowest point of circulating platelets. *onset of neutropenia. | |
| Myelosuppresson management | hand Hygiene |
| Colony stimulating Factors (CSF’s) patients given pegfilgrastim to increase blood. | |
| Sae food handling- avoid raw, uncooked foods | |
| Keep plants out of patient rooms | |
| Prevent trauma to skin and mucosal integrity | |
| Perform oral care | |
| Avoid family and friends with cold and flu | |
| Get flu vaccinations | |
| Caution with Pet care | |
| Monitor temperature and notify LIP if fevers | |
| Monitor lab cultures for bacteria identification and sensitivity. | |
| Fatigue | Most common and long lasting side effect of QOL and ADL |
| Fatigue scale | |
| recurrent progression of disease | |
| current medications- analgesics, antiemetics, sleep aids | |
| ROS- malnutrition, insomnia, anxiety, depression, activity, pain, nausea, emesis | |
| Onset, pattern and duration of fatigue | |
| Collaborative management and family education | |
| non-pharmacologic | |
| Nausea and vomiting | Determine the risk factors: single agent vs combination chemo, , metabolic |
| physical: GI obstructin, constipation, cranial pressure, anticipatory nausea | |
| psychological | |
| metabolical- renal failure, hypercalcemia, constipation | |
| Pharmacologic management: serotonin antagonists, NK-1 Antagonist, corticosteroid, | |
| Dopamine antagonists, Anxiolytic. | |
| Nonpharmacologic management | |
| Patient/Family education | |
| Diarrhea and constipation | Determine risk factor: |
| Chemo/biotherapy?targeted agents | |
| Radiation therapy- external beam and brachytherapy | |
| Immunosupressants/Neutropenic sepsis | |
| Diet/Inflmmatory conditions/Malabsorption/Anxiety/Stress | |
| Nausea/Vomiting | |
| Impaction/Ileus | |
| Hemorrhoids | |
| Assessment: | |
| Pattern of elimination | |
| Level of activity | |
| medications | |
| Radiographic studies | |
| Abdominal pain/cramping | |
| Abdominal/rectal exam | |
| Characterisitc of Last BM: quality, formed | |
| Diarrhea Management: | |
| Monitor Stool number, amount, consistency | |
| Replace fluid and electrolytes | |
| administer antidirrheal medications | |
| Patient/family education | |
| Constipation management: | |
| Laxative options | |
| Non-pharmacologic interventions | |
| patient/family education | |
| Anorexia | the abnormal loss of appetite for food that can result in loss of adipose and muscle tissue. |
| Pathophysiology- change in taste of food, metabolic, tumor on gastro-intestinal tract. | |
| Risk factors: | |
| Advanced tumor- gastro-intestinal, Lung | |
| Solid tumor | |
| Chronic Illness= CHF, Pulmonary disease | |
| Multimodal Therapies | |
| Clinical manifestations- involuntary weightloss greater than 5%. | |
| Patient/Family Education- dietary consults, supplementation | |
| Mucositis: | Risk factors, Clinical Manifestations, Oral assessment. |
| Management: Prevention, Treatment, Hygience program. | |
| Changes in Taste, difficult swallowing.Edemas, ulceration. | |
| Alopecia | Most visible sign. Head, eyebrow, eye lash, pubic hair. |
| Risk Factors: | |
| Agent received | |
| High dose Chemotherapy | |
| Comorbidities | |
| Nutrition Status | |
| Radiation therapy | |
| Clinical Manifestations- expercted time frame to Alopecia | |
| Patient/family education | |
| Chemo Brain | Cognitive changes based on therapy: concentration, attention, language, motor skills, learning |
| memory. Stress, anxiety, depression. | |
| Risk Factors: Age, psychological factors, fatigue, | |
| Regimens: multimodal, dose intensity, cumulative effects | |
| Patient family education: acknowledge and validate, practical solutions. | |
| Neurotoxins, white matter damage to brain, Dna damage, cytokine increae, hormonal | |
| Increase sleep intervals, regular exercise, regimented daily planning. | |
| Goal of chemotherapy | Cure: prolonged absence of disease |
| Control: preventing the growth of cancer cells without the complete elimination of disease | |
| Palliation: comfort measures and/or reduction in side effects and symptoms. | |
| Principles of Cancer therapy | Adjuvant: therapy following primary treatment (surgery, RT) |
| Neoadjuvant: use of one or more treatment modalities prior to primary therapy | |
| example: chemo or radiation before surgery. | |
| Chemoprevention: treatment ot prevent cancer in high risk patients. | |
| Myeloablation: Obliteration of bone marrow in preparation for Stem cell or bone marrow transplant | |
| Combination vs Single agent therapy | Combination of agents with different mechanisms of action is able to increasee the |
| proportion of cells killed at any one time. | |
| Combination chemo reduces the possiblilty of drug resistance. | |
| Agents used in combination chemotherapy have proven efficacy as single agents. | |
| Measuring tumor response | CR: Complete response- removal of tumor confirmed after one month. |
| PR: Partial response- half mass gone in one month. | |
| SD stable disease- reduction of tumor mass is less than 50%.<25% increase in new tumor growth. | |
| PD progressive disease- 25% growth in new disease and or new tumors. | |
| Relapse: a new tumor appears or original tumor reappears. | |
| Dosing Chemotherapy | Most cytotoxic chemotherapy drugs are dosed based on BSA (body surface aea). |
| BSA is the estimated total area of a persons skin expressed in square meters (m2). | |
| BSA is calculated using current and accurate height (cm) and weight (kg). | |
| Patient Education | Ensure patient and family understand meaning of “cycle” in chemotherapy. |
| usually chemo 2 cycles every two weeks, twice per months, or 6 months thereafter. | |
| Total of 12 cycles. | |
| Avoid interruption in treatment cycles, planning around vacations and events. | |
| Encourage participation in care. | |
| Explain diagnosis and treatment | |
| Explan potiential side effects of treatment | |
| Explain signs and symptoms to report | |
| identify available resources | |
| Biotherapy | Biologic therapy and Immunotherapy |
| Purpose: uses the body’s own immune system to fight cancer | |
| and to reduce treatment-related side effects. | |
| Help cells damaged by treatment, reprogram cells. | |
| MoAbs )Monoclonal antibodies) | Produced in lab: designed to bind to the antigens on malignant cells |
| Block the growth of the tumor and/or recruit the body’s immune system to attack cancer cells | |
| Can be given as a montherapy, in combination with chemotherapy, and with other targeted | |
| therapies under clinical trial. | |
| Types of MoAbs | Human- umab |
| Murine- momab (mouse) | |
| Chimeeric – ximab (human and mouse) | |
| Huamnized -zumab (human and mouse) | |
| Mechanism of action | Specific protein binds to specific receptor on cell surface |
| When antibody binds to recepto, all downstream signaling is halted. | |
| Cell apoptosis | |
| Monitoring patient on MoAbs | Hypersensitivity Reactions |
| Aggressive IV hydration | |
| Monitoring electrolyte imbalance every 6 hours and replacements as needed. | |
| Monitor cardiac status as required | |
| Acneform rash.(not acne, nor do not use acne OC drugs, just report to doctor) | |
| Surgery- | localized |
| preventive | |
| diagnostic | |
| Staging | |
| Debulking | |
| Curative- mastectomy example | |
| Palliative- repair of a side effect | |
| Surgical complications | Pain, Atelectasis (inadequate breathing) |
| Blood clots, fatigue, muscle atrophy, anesthesia effects, confusion, infection. | |
| Radiation therapy- | High dose of radiation to kill cancer and stop spread |
| routes: external beam, internal | |
| 60% of patients get radiatin to treat and reduce symptoms | |
| Transplants | hematopoietic stem cell, Bone marrow. |
| Myeloablative and Nonmyeloablative | |
| Allogeneic- donar. Luekemia, lymphoma, myeloma, aplastic anemia, thalassemia, immune def. | |
| Autologous- self. Hodgkins, non-hodgkins, myeloma, testicular. Stem cell harvest. cytoxan. | |
| Cord Blood- umbilical cords and placenta |
| Breast Cancer | > 1 million breast cancer new cases. Global health burden. |
| Most common in USA women 240,000 new diagnoses expected in 2014 | |
| >40,000 deaths from breast cancer in US each year. | |
| Most frequently diagnoses cancer amoung women each year. | |
| Incidents increase with age and peaks between | |
| 2nd leading cause of cancer death in women in the US. 15% in 2010. | |
| Death rates have declines since 1991 by more than 30% due to early detection and treatment. | |
| 2005 Berry NEJM study shows that from 1975 to 2000, the rate of death was lowest per 100k women: | |
| If they had Screenings and Adjuvant Therapy. Survival was lower with just one or none. | |
| Adjuvant as chemotheraoy, Hormone therapy, Anti-body therapy, and Radiation treatments. | |
| Declining Deaths | Early detection yields more but small tumors |
| Better therapy: Broadened use of Tamoxifen, AI’s, (Aromatase inhibitors) | |
| Surgery, and Antiresorptive bone agents. Chemotherapy. Trastuzumab, Radiation. | |
| Good news: incidents and mortality decline, early diagnosis is cureable. | |
| Challenges: Early stage breast cancer can still have distant recurrence, | |
| metastatic breast cancer is treatable but not cureable. (Stage IV) | |
| Breast Cancer: | normal ducts begin to have Atypical Hyperplasia, then DCIS, (Ductal Carcinoma in situ) |
| lastly cancer invades other tissue. Invasive ductal Carcinoma. | |
| Risk Factors: | Gender, age, Race, Genetic (BRCA1, BRCA2), personal history of breast cancer |
| Early menses and or late menopause, hormone therapies, late or no pregnancies, | |
| family history, dense breast tissue, Lifestyle: alcohol, smokng, obesity, exercise, diet. | |
| BRCA testing | If known mutation in the family, close relative with breast cancer <35 yo, |
| multiple early onset or bliateral breast cancer, ovarian or fallopian tube cancer, pancreatic cancer, | |
| ashkenazi jewish ancestry, any history of cancer in family. | |
| Detection | Mammogram year age 40 and up. |
| Clinicla breast exam- every 3 years before age 40, annually after 40. | |
| Breast self exams, ultrasound, Breast MRI | |
| Biopsy | Fine needle aspiration- remove fluid from cyst. |
| Core needle biopsy- blind, image guided, sterotactic, cells removed from lump with needle. | |
| surgical biopsy- tissue removed. | |
| Staging | tumor size, local or multiple lymph node metastasis |
| Are brain, lung, liver, bone affected? | |
| 0- small, no lymph involvment, no spread, survival 100% | |
| I- 2cm, No lymph, no metastasis, 96% survival | |
| II- 205 cm, yes or no lymph, No spread, 84% survival | |
| III- >5cm yes lymph involvement, No spread, 52% survival. | |
| IV- metastasis yes, survival 24%. | |
| Treatment strategies: | Early- surgery, XRT (radiotherapy)-systemic, goal is to cure. |
| Locally advanced- systemic, surgery, XRT, , cure and improve local control | |
| Metastatic- systemic and XRT, palliative treatment. | |
| Modular substyles: | HR+/HER2- (luminal A) 505, indolent (bone, soft tissue), tx: endocrine agents |
| HR+/HER2+ (luminal B) 10-15%, aggressive (visera), tx: antiHER2 and endocrine agents, chemotherapy | |
| HER2+/HR1 (HER2+), 10-15%, very aggressive (viceraa and CNS), antiHER2 agents and Chemotherapy | |
| Triple Negative (basal-like), 20%, very aggressive (viscera and CNS), Chemo and platinums promising | |
| BRCA 1 or 2 mutation, <5%, moderately aggressive, chemo (platinums) and PARPi promsing. | |
| Theraputic options and outcomes | Chemo: ER/PR negative, visceral mets, faile dendocrine therapy |
| Endocrine: ER and/or PR postive | |
| Trastuzumab, Pertuzumab, TDM-1, Lapatinib: her2/Neu-postive | |
| Bevacizumab: HER2/Neu-negative, first-line therapy | |
| RANKL inhibitors, Bisphosphonates: Osteolytic bone mets | |
| Selected Toxicities with therapy | |
| endocrine therapy- hot flashes, vaginal dryness or discharge | |
| Bevacizumab- hypertension, throbembolic disease | |
| Trastuzumab- Cardiac Dysfunction | |
| Lapatinib- diarrhea, dermatologic | |
| cytotoxic agents | Anthrocyclines- caridomyopathy, alopecia |
| Paclitaxel- neuropathy, alopecia | |
| Docetaxel- fluid retention, hyperlacrimation | |
| Ixaqbepilone- neuropathy, fatigue | |
| Eribulin- neuropathy and fatigu | |
| vinorelbine- Obstipation, neuropathy | |
| Capecitabine- hand-foot symptoms, diarrhea | |
| Gemcitabine- fever, flu-like symptoms | |
| Metastatic Breast Cancer (MBC) | Balance Efficacy (survival) vs Toxicity (minimal toxicity) |
| Take into consideration Disease characteristics and patient characteristics. | |
| ER/PR+: hormonal-treatient patient- first line, second line, and third line hormonal treatments. | |
| ER/PR-: chemo related: HER+ based chemo, first, second, and thrid line | |
| Triple negative ER/PR, HER-: chemo first, second and third line. | |
| HER- (ER/PR+): chemo, first, second, and thrid line. | |
| Trastuzumab- essential part of Rx of HER2+ MBC. Chemo plus Trastuzumab decreased cancer progression. | |
| Marine sponge Halichondria Okadai (Eribulin Mesylate, E7389) target agent, blocks mircortubule. | |
| MBC median survivial is 3 years, incruable, but tx is to extend life and qulity of life. | |
| MBC- hormonal therapy is tolerated and frequently recommended for women whith hormone | |
| responsive MBC andnot at risk for visceral crisis. | |
| Chemo is for women with hormone-refractory disease, hormone receptive negative disease, | |
| rapidly progressive or significant cancer-related symptoms. | |
| MBC treatment considerations | Age, preference, co-morbid conditions, performance status, ER/PR status, HER2 status, |
| disease-free interval, prior adjuvant therapies, number and distribution of metastatic sites, | |
| potiental of viseceral crisis, Bone metastases need biophosphanate therapy, Palliative XRT for pain. | |
| Early stage Breast Cancer | Breast Conserving- cancer and local nodes removed in axillary |
| Simple Mastectomy- breast and local nodes removed in axillary | |
| Modified Radical Mastectomy- all removed. | |
| Pathology | In Situ: ductual carcinoma in Situ and Lobular carinoma in Situ. Benefit is local control. |
| Inflitrating Carcinomoa- infiltrating ductal and invasive lobular, Benefit: systemic control. | |
| systemic recommendations | Axillary nodes, tumor size, histologic grade, Estrogen and progesterone receptiors HER2/neu status. |
| Oncotype DX 21 gene recurrence score | low risk: RS < 18 |
| Int rist RS >18 <31 | |
| High risk >31 (benefit from chemotherapy) | |
| Adjuvant Chemo regimens | CMR- cyclophosphamide, methotrexate, fluorouracil |
| AC- doxorubicin, cyclophosphamide | |
| CAF/FAC: doxorubicin, cyclophosphamide, flourouracil | |
| FEC/CEF: epirubicin, cyclophosphamide, flourouracil | |
| A->CMF: doxorubicin, cyclophosphamide, methotrexate, flourouracil | |
| AC- Paclitaxel | |
| Emerging therapy PARP | PARP as a target, key regulator of DNA damage repair, binds directly to DNA damage and |
| produces large branched chains of poly (ADP-ribose) | |
| it is differentially upregulated in primary breast cancers including ER-, PR-, and HER2- subtypes. | |
| Lung Cancer | |
| Epidemiology | 2nd most common cancer in Men and Women, Number one in death in both |
| Causes and risk factors | Tobacco smoking, 85-90% of all lung cancer-related deaths. |
| Smokng cessation: former smokers who had quit >15 years had 80-90% decrease risk versus current smokers. | |
| former smokers continue to have a 10-80% higher risk than never smokers | |
| Ongoing smoking by early stage patients have increased likelihood of all-cause mortality, tumor recurrence, and | |
| development of a secondary primary tumor. | |
| Second hand smoke- 15-35% of lung cancers due to second hand smoke, increased risk if exposed prior to age 25. | |
| Occupation/environment: asbestos, radon, cooking from coals. | |
| Benign Lung disease- COPD, chronic bronchitis, pneumonia, tuberculosis | |
| Radiation: breast and hodgkins disease patients have increased risk | |
| Lung Cancer screening | NLST (National Lung Screening Trial) 2013 data: |
| The 3 year trial, enrolled asymptomatic participants age 55 – 74, 30 pack-year history. | |
| Randomnized to low dose CT vs. chest Radiography | |
| Conclusion: although there was low positive predictive value with low dose CT, | |
| more early stage cancers were detected as compared to chest radiography. | |
| Role as mid-level practitioner | Clinic, Operating room, post-operative floor |
| History, physical exam, findings, plan. Mid-levels allow for great amount of patients to be seen in clinic and operating room. | |
| It provides more provider-patient face time as visits are split between attending NP/PA. | |
| Helpful in academic setting with assisting in education of rotating fellows and residents. | |
| Cliic presentation | SX: couth, weight loss, dyspnea, chest pain, hemoptysis, bone pain, hoarseness. |
| Symptomatic patients often represent advanced stage of disease. | |
| Early lung cancers are often found incidentally. | |
| Metastatic disease of primary lung cancer: common sites- brain, bone, liver, adrenals, skin | |
| sx: weight loss, fatigue, night sweats, loss of appetite. | |
| Diagnostic imaging | chest x-ray, CAT scan |
| example: Squamous cell CA (cancer) RLL CXR in rt. Lower lobe | |
| AdenoCA in Situ. downward scan. | |
| diagnosis and Staging | Most imporant part |
| Role of CT surveillance: if nodule found, wait, they may have infection or inflammation, try antibiotics first and rescan 6 weeks. | |
| Work ups: | |
| Biopsy: CT guided vs. VATS wedge. If not shrinking.biospsy to pathologist.VATS: video assisted thoracic surgery biopsy. | |
| Recent CT scan, with IV contrast is best. IV contract to see if vessles are attached to tumor. | |
| PET Scan- show if nodule is lighting up. If spreading, or gone to lymph nodes. If lymphs are medial or distal, determine treatment. | |
| MRI Brain- more useful in stage II or higher. PET scans only scan neck down, MRI needed for brain. | |
| Other testing for pre-operative risk assessment: | |
| Pulmonary function tests | |
| VQ scan | |
| Cardiac risk evaluation | |
| Types of Lung CA: NSCLC vs SCLC | Non-small cell carcinoma vs Small cell carcinoma |
| Histology Data: | |
| Ademonocarcinoma: 38% | |
| Squamous cell 20% | |
| Large Cell 5% | |
| Small Cell 13% | |
| NSCLC NOS 18% | |
| Other 6% | |
| Pathology Data: | |
| Large cell 2% | |
| Adenosquamous 1% | |
| Adenocarcinoma 72% | |
| Squamous cell 25% | |
| Increasing incidence of adenocarcinoma with corresponding decrease in other NSCLC and SCLC. | |
| TNM Staging | Metastases: M0: absent. M1: present |
| Lymph Node (N). N0, N1, N2, N3. +positive, -negative in following regions: | |
| Supraclavicular | |
| Scalene (ipsi/contralateral) | |
| Mediastinal (ipsi/contralateral) | |
| Subcarinal | |
| Hilar (ipsi/contralateral) | |
| Peribronchial (ipsilateral) | |
| Stage 0 | No Tis (Carcinoma in situ) N0 (no lymph nodes affected), M0 (metastasis absent). |
| Criteria | Primary Tumor (T) a. size, b. endobronchial location, c. local invasion, d. other |
| Stage 1A, Stage Iia | T1, a,b,c, no invasion proximal to the lobar bonchus, surrounded by lung or visceral pleura. |
| < 3 cm | |
| Stage Ib, Stage Iib | T2: a.b.c.d , main bronchus, viseral pleura, atelectasis (collapse), obstructive pneumonitis, hilar region, but not entire lung. |
| > 3 cm | |
| Stage Iib | T3 (a and c)/b/d. main bronchus, chest wall, diaphragm, mediastinal, pleura, pericardium, atelectasis, entire lung. |
| any size | |
| Stage IIIb | T4: (a and c) /d. mediastinum, treachea, heart, great vessles, esphagus, vertebral body, carina (cartilage of branchia) |
| Malignant pleural, pericardium effusion, , satellite tumor, ipsilateral primary tumor lobe of lung | |
| any size | |
| Stage IV | M1 (and T, any N) |
| Treatment | |
| Stage I | surgery |
| Stage II | a lymph is involved, surgery, tumor and lymph node, systemic chemo in some cases. |
| Stage III | 7 cm and several lymph nodes |
| TX: no single approach, surgery with chemo, chemoradiation | |
| Stage IV | tumor on both lungs, lymph involvement, spread to none, brain, liver, adrenal |
| tx: chemotherapy, palliative radiation therapy. | |
| NSCLC: Non surgical management | Radiofrequncy ablation- fry the cells. Radiatin therapy: EBRT, SBRT, chemotherapy- single agent, combination, targeted. |
| Platinum agents (cisplatin, carboplatin), taxanes, (paclitaxel, docetaxel). | |
| Combination therapy (Bevacizumab, Crizotinib, Cetuximab) | |
| Operating room | PA/NP role: operating oppoiste attending and fellows, responsible for post op orders. |
| Smaller staging precdures: EBUS-TBNA or Endobronchial ultrasound, Transbroncial needle aspiration | |
| mediastinoscopy | |
| Major lung recection operations: minimally invasive versus open wedge resection, | |
| segmentectomy, lobectomy, pneumonectomy. | |
| Mediastinoscopy | classic stagin procedure that uses small incision at sternal notch, can sample paratracheal and subcarinal lymph nodes, low M&M, |
| 100% specificity, higher sensitivity when preceded by CT/PET. | |
| Useful when larger samples are necessary, molecular profiling, lymphoma. | |
| EBUS-TBNA | Real-time imaging of peri-bronchial structures and needle biopsy of lymph nodes. |
| Access to paratracheal subcarinal and hilar LN. Better accuracy, less time, fewer biopsies. | |
| Major operations | VATS, Open thoractomy, Robotic assisted VATS |
| Lung wedge resection- for suspicious nodule, can proceed to lobectomy if malignant, most often perfomred VATS. | |
| Segmentectomy, lobectomy: anatomical resection of lung lobe or segment of lobe. Receommended for early | |
| stage tumors, NSCLC stage I and II. Can be performed via open thoracotomy, VATS, pr robotic VATS. | |
| Thoracotomy morbidity 45%, mortality 3.6% | |
| VATS morbiditiy 28%, mortality 0%. | |
| Lobectomy vs limited resection | wedge resection not recommended for stage 1 patients. Lobectomy still best surgery for overall survival in good risk patients. |
| Segmentectomy reasonable for tumors <2cm. Lobectomy for tumors > 2 cm and stage 1. | |
| High risk patients should be considered for segmentectomy regardless of tumor size. | |
| Pneumonectomy | removal of entire lung, must be strongly clincally indicated and patient must have pulmonary reserve. |
| Significant mortality between 5-10%. Reasonalbel for certain T3 and T4 tumors without nodal disease. | |
| Indications: Proximal bronchial tumor. Adjactent to right upper lobe orifice. Tumor extends across major fissure. | |
| Prior resection of other ipsilateral lobes resulting in completion pneumonectomy. | |
| Malignant pleural effusions (Iv) | Pleurodesis- scarring of parietal pleura so as to form adhesions. |
| insertion of pleurx catheter-drain the effusion. Patients can learn how to drain at home. | |
| Post-op floor care | Prevention, early identification, early treatment of cardio-pumonary complications |
| Most complications occur within first 3 post-op days. | |
| Monitoring: | consciousness/alertness- inappropriate analgesia, hypoxia? |
| Fast or shallow respiration, underlying atelectasis? | |
| Daily CXR- as long as chest tube continued | |
| Chest tube: airleaks? Amount? Bloody? Milky? | |
| Periodic assessment of wound dressing. | |
| Hemodynamics essential to status of patient: HR, BP, UOP, O2 saturation. | |
| Prophylactic interventions for thoracic surgical complications: pain control, deep breathing exercises, effective cough, ambbulation. | |
| Pneumonia risk.fevers, WBC, mucus. Sputum culture, cephalosporin ABX. | |
| chest PT, POPP patient education for post-op risks and complications. | |
| complications | Cardia arrhythmias: AF, atrial flutters, paroxysmal atrial tachycardia. |
| tx: low does RTC IV metoprolol or Dilt gtt. Patients with cardia history, older than 65. | |
| Prolonged air leaks and post-op spaces- can dissipate within 1 week. | |
| Empyema- infected loculated parapneumonic effusion. CT to evaluate, ABX therapy and drainage. |
| Prostate Cancer | Many men will get prostate cancer 14% of all new cancer cases in US |
| A fraction of these men will die of the disease, or suffer from it. | |
| It is the second leading cause of cancer related death in American Men. | |
| Minority men have a higher risk. | |
| Overtreatment- incompetence and erectile dysfunction | |
| PSA screening: PSA is not cancer specific, only prostate specific. Benign prostate issues occur, just not cancer. | |
| Specific overlap between BPH and cancer | |
| natural biological PSA variations: | Patient age and prostate volume |
| Prostate cancer | |
| Prostatic inflammation | |
| Race/ethnicity | |
| Screening paradox | Increase detection rate but did not prevent deaths. 22% more cancer in the screening group. |
| Family history of prostate cancer should be considered. | |
| Risk assessment: death from prostate cancer, death from other causes, Quality of life- over and under treatment | |
| Risk of disease are gauged by: stage, Gleason score, PSA. | |
| Staging | T1 |
| T2 | |
| T3 | |
| T4- invading other structures | |
| Bone disease | Is the central issue of treating metastatic prostate cancer |
| Primary source of morbidity and mortality | |
| It is the most feared complication of cancer: cord compression, marrow failure, pain, fracture, death. | |
| Gleason Score | Grade 1 to 5. Dominate and lesser population. Example 4+4 + 8. |
| Paradox of reasonable choices | surveillance- serial monitoring of the cancer without treatment |
| radiation therapy- external beam or seed placement | |
| Hormones or no hormones | |
| Surgery: radical prostatectomy | |
| High risk disease | Risk of treatment failure regardless of modality |
| Risk of metastatic disease and risk of death. | |
| High Gleason score does not need surveillance, they need treatment to prevent spread. | |
| Hormones | Testosterones and DHT are fuel for prostate cancer growth. |
| Hypothalamus- LHRH – pituitary- ACTH to adrenals and FSH and LH to testes. | |
| Adrenals- androstenedione DHEAS, DHEA- testosterone, Estradiol | |
| Testes- androstenedione testosterones (T) and Estradiol. | |
| Adrenals and testes- SHBG, (T) 5 alpha reductase- DHT – AR- Protein synthesis- Prostate cell. | |
| Flutamide Bicalutamide Nilutamide- inhibit testosterone and androgen receptor. Enzulutamide | |
| Ketoconazole- reduce testosterone in adrenal and testes and tumor. Arbiraterone. | |
| Orchiectomy Ketoconazole- | |
| Finasteride- reduces 5 alpha reductase. | |
| Leuprolide Goserelin- LHRH production reduce drug. GnRH antagonists | |
| Prostate Cancer Clinical states | Castration Sensitive- |
| clinically localized disease -> Rising PSA: castration sensitive-> Clinical metastases or Rising Castrate Resistant | |
| Castration Resistant- | |
| Rising PSA: castrate resistant- > Castration sensitive metastatic _. Castration resistant 1st line -> mCRPC 2nd line. | |
| Progressive prostate cancer | No Cancer-> Localized disease -> Rising PSA -> Castrate sensitive metastatic -> CRPC metastatic |
| tx: lower testosterone agent at localized disease stage. | |
| Early vs Defeered hormones | MRC- primary therapy for localized /met |
| Messing- adjuvant, N1 | |
| Bolla- adjuvant, high grade T3, 4 | |
| 85-31- adjuvant, T3 or N1 | |
| Early Hormones | Early bisphosphonates for bone wasting |
| Early therapy for impotence | |
| Early SSRI’s for hot flash and depression | |
| Early Breast RT for gynecomastia | |
| Early cholesterol and glucose and weight management | |
| Intermitten Hormal therapy | PSA high 45_> lower to 0 with hormone therapy- > take a break -> if psa gets up like 20 range _> repeat hormone therapy. |
| do chemo and radiation while on hormone T blockers if PSA is high again. | |
| Castration resistant | resistant to testosterone lowering agents. |
| It is still exquisitely sensitive to testosterone and DHT. | |
| Adrogen receptor (AR) | receives hormones that fuel the growth of cancer tumor by way of either AR mutations, AR overexpression , |
| or copious androgens within the tumor. It might be adrogen sensitive, or finding other sources of androgen in the body. | |
| Reduce the adrogen abiraterone | Cholesterol with Desmolase |
| Pregnenolone-> progesterone-> deoxy-corticosterone -> Corticostero -> Aldosterone | |
| CYP 17a-hydroxylase for Pregnelone | |
| 11b-hydroxylase for Deoxy-corticosterone | |
| 17a-OH-pregnenolone -> 17a-OH-progesterone -> 11-Deoxy-cortisol ->Cortisol | |
| c17, 20-lyase to block 17a-OH-pregnenolone | |
| DHEA -> Androstenedione -> testosterone -> DHT or ESTRADIOL | |
| CYP19: armomaatse to stop DHT and Estradiol | |
| Abiraterone and mCRPC | abiraterone 1000mg daily and prednisone 10 mg daily |
| hormonal therapy could prolong survival in men with metastatic castration resistant disease by 35% | |
| AR overexpression | Enzalutamide |
| Enzalutamide is an oral investigation drug rationally designed as a new hormonal agent to target androgen receptor (AR) signaling, | |
| a key driver of prostate cancer growth. | |
| Enzalutamide- first in new class of AR signaling inhibitors that affect multiple steps in the androgen receptor signaling pathway. | |
| Enzalutamide for mCRPC | mCRPC- Castration resistant prostate cancer |
| mDV3100- 180 mg daily vs. | |
| Enzalutamide 160 mg daily. Overall survival was higher with this drug. | |
| good for both pre and post chemotherapy. Risk reduction for death. | |
| Alliance A031201 | Enzalutamide 160 mg, Abiraterone 1000mg, prednisone 5 mg |
| Hormones for prostate cancer | AR is active thought the natural history of the disease. |
| “Hormonal therapy” covers a band swath of anti-AR approaches- survival data for both castration sensitive/resistant disease/ | |
| Both ligand reduction and anti-AR approaches | |
| No other modality has had as broad an application or as clinically beneficial results for such a large group of patients. | |
| Bone tumor | pain, fracture, disability, blood dyscrasias, neurologic compromise, death. |
| deposited calcium and phosphate crystal on new bone, bone deposition, new layers of bone where the cancer is. | |
| new bone gets over deposited. | |
| Radium-233 targets bone metastases | radium 233 acts as a calcium mimic. It is a earthy element on the periodic table. |
| Naturally targets new bone growth in and around bone metastases | |
| Radium 233 is excreted by the small intestines. | |
| Low rate of damage to the bone and marrow, increases quality of life with little or no side effects. | |
| Immunotherapy | Sipuleucel-T: WBC from blood, collected and exposed to prostate proteins and injected into prostate. |
| It is a kind of vaccine therapy. | |
| Chemotherapy | Taxanes. Taxus baccatus. |
| Cabazitaxel | |
| Docetaxel | |
| Many men will go right to chemo if disease is first found to be metastatic. Then hormone therapy is introduced. | |
| Conclusion | Prostate cancer represents a wider spectrum of risk than most other cancers |
| Good decision making relies on a adequate understanding of risk of disease, risk of therapy, and risk of patients other diseases. | |
| Substantial advances in what was previously an untreatable condition, mCRPC, now is substantially bending the | |
| survival curve of prostate cancer. Improving overall survival and quality of life. |
| Gynecological Cancers | normally done by gynecological surgeons with chemotherapy |
| MSK- separate surgeons and medical oncologist | |
| Gynecologic Cancers- New cases | 15% Uterine Cervix |
| 2014 study | 56% Uterine Corpus |
| 23% Ovary- *diagnosed late and not curable | |
| 5% Vulva | |
| 3% Vagina | |
| Death Rate: | 14% Uterine Cervix |
| 2014 study | 30% Uterine Corpus |
| 49% Ovary* | |
| 4% Vulva | |
| 3% Vagina | |
| Ovarian Cancer | Age, Family Hx (BRCA-1 (80-90% risk), BRCA-2), |
| Ovarian Hx (Age of menarche, Use of birthcontrol (OCP oral contaceptive), Gestational Hx, age of menopause) | |
| BRCA- removal of ovaries age 35 and up. | |
| OCP and having babies decrease risk. | |
| Origin | Tubes, presentation: insidious, non-specific |
| bloat, change in bowels, urinary frequency, delay in diagnosis. | |
| Dx: CT scan and Biopsy/Surgery if suspected. | |
| Surgery | Staging and debulking (remove as much of tumor as possible) |
| Midline Laparotomy_. Hernias | |
| Surgical gynecologic oncologist | |
| Optimal vs sub-optimal | |
| Upfront (surgery right away) vs Interval (chemo then surgery) | |
| Secondary, tertiary (additional surgeries later) | |
| Stage | Stage I- just in ovary |
| Stage II- spread to pelvis | |
| Stage III- spread into abdomen | |
| Stage IV- Liver, Lungs | |
| 75-80% are diagnosed at stage III/IV | |
| Histology (Ovarian cancer types) | 75% high grade Serous |
| Endometroid | |
| Low grade Serous | |
| Clear Cell | |
| Ovarian Cancer Chemo | 6 cycles: Taxol or Docetaxel. Once every three weeks. |
| then: Carbo or Cisplatin (paltinum). (2 different drugs will be used like taxol, then carbo) | |
| IV vs IP (this port goes to abdomen) | |
| Mediport- a port direct into the veins | |
| After chemo then what? | Remission/Replapse/Resistance |
| Primary therapy- cure: complete remission. | |
| Primary therapy- refractory/persistent disease. (Grave prognosis) | |
| Remission- chemotherapy | |
| Resistance to chemotherapy- | |
| Relapse | Rarely curable, survival for many years |
| Many rounds of chemo with side effects: neuropathy, chemo-brain, diarrhea, constipation, fatigue. Alopecia, rash. | |
| Repeat surgeries- hernias, bags, tubes. | |
| Fatigue- chemo, anemia, lack of sleep. Chemo-brain- forgetful, depression, losing items, etc. | |
| Chemo- | Carbo-Taxol:side effect: make WBC, RBC count lower, causing anemia and fatigue. Bowles, hairloss, neuropathen. |
| Liposomal Doxorubicin: hand-foot, mucositis | |
| Hand foot syndrome- drying, peeling of hands and feet. Mucositis- dry mouth. | |
| Topotecan: Fatigue, Cytopenias | |
| Cytopenias (more than one kind of anemia, low blood cell count) | |
| Gemcitabine- fatigue, cytopenias, fever, inflammation | |
| Bevacizumab- sorethroat, nose bleed, headache | |
| Ovarian cancer complicaitons | Clots, DVT, PE (pulmonary embolism) |
| Edema, Ascites (fluids in abdomen), Effusions (fluids around lungs) | |
| Bowel Obstruction. Colostomy, Ileostomy, Stent. Drainage PEGs | |
| Kidney blockage | |
| Brain METS | |
| Liver Failure | |
| Lung METS | |
| Ovarian cancer consequences | Pain, fatigue, malnutrition, Depression/anxiety, economic/work, social/sexual, physical/cognitive impairment |
| effects on caregivers/families, disability, death. | |
| Cervical Cancer | average age 48, Hi risk is HPV, tobacco, HIV+ |
| PAP smear screen reduces risk. | |
| HPV- cervix cancer, Oropharynx cancer, Anal cancer, Vulva cancer, Vaginal cancer, penis cancer. 32,000 per year. | |
| HPV vaccines | Gardasil – recombiant VLP: capsid protein L1 |
| HPV 16,18 (70% CxCa and some H and N) | |
| HPV 6,11 (90% Genital warts) | |
| Cervarix- recombiant VLP: capsid protein L1 | |
| As04 Adjuvant, HPV 16,18 (70% CxCa and some H and N) | |
| Girls routine 3 does age 11-12, catch-up vaccine age 13-26 | |
| Boys age 9-21 | |
| Origin | CIN-III |
| Presentation- abnormal PAP, bleeding, pelvic pain, Urinary Sx. | |
| Staging | Ia,b: at cervix |
| IIa,b: getting into surrounding tissue like vagina or outside cervix (parametrial tissue). | |
| IIIa,b: getting into surrounding tissue outside cervix, pelvic floor, bone, pelvic sidewall. | |
| IVa,b: moving into rectum and more. | |
| work-up: bimanual, EUA, PET/CT, MRI | |
| Urine cytology, Renal U/S. | |
| usually chemo and raditation without surgery. | |
| surgery | Radical Hysterectomy |
| Trachelectomy | |
| Radiation | Pelvic radiation 28x external beam and brachy |
| side effects: fatigue, diarrhea, cytopenias, cystitis, lymphedema, colitis, second cancers (rectal, leukemia), nausea/vomiting. | |
| 5 1/2 weeks daily. | |
| Cisplatin with RT | fatigue, constipation, nausea/vomit, cytopenias, electrolyte disturbances, Ototoxicity, Dehydration, kidney damage |
| tinnitus, hearing loss. | |
| Relapse | Less response to chemo. |
| Complications | Pain, clots, DVT, edema, bowel obstruction, kidney blockage, ureteral stents, Lung Mets. |
| Consequences | Pain, fatigue, malnutrition, Depression/anxiety, economic/work, social/sexual, physical/cognitive impairment |
| effects on caregivers/families, disability, death. | |
| Enometrial Cancer | Type 1: Obesity, DM-2, Estrogens, Tamoxifen |
| Type -2: Genes HNPCC, BRCA-1, Tamoxifen | |
| Staging | Type1: post-menopausal bleeding (PMB), , typically found early |
| Type 2: PMB or Mets, can metastasize quickly | |
| Stage I: uterus lining | |
| Stage II: uterus lining and into connecting tissue | |
| Stage III: uterus, connecting tissue, cervix | |
| Stage IV: uterus, into fallopian tube, and ovaries, ligaments more. | |
| Surgical- | removal of uterus and tubes, lymph node sampling |
| Omentectomy, tumor debulking, washings. | |
| Adjuvant RT and or chemo- depends on stage and aggressiveness. | |
| Radiation: IVRT (bradytherapy), WPRT (External beam) | |
| Chemo: +/- Cisplatin with RT. | |
| chemo only: Taxol and Carboplatin | |
| Recurrence | Radiation: WPRT , if limited to pelvis and no prior RT |
| Chemo- metastatic disease, non-curative, carbo-taxol, Bevacizumab, Anthracyclines. | |
| Hormonal therapy | Megesterol- blood clots, weight gain, hyperglycemic |
| Tamoxifen | |
| Aromatese inhibitors | |
| Complications: | Clots, Edema, bowel obstruction, Kidney blockage, Liver failure, Lung mets, Bone mets |
| Consequences: | Pain, fatigue, malnutrition, Depression/anxiety, economic/work, social/sexual, physical/cognitive impairment |
| effects on caregivers/families, disability, death. | |
| Rare gynecologic cancers | Vaginal, Vulva, Sarcoma, Carcinosarcoma, germ cell, GTD, Small Cell, Granulosa Cell. |
| Supportive Care for Cancer patients | |
| Integrative Stratagies | anxiety, stress, chemo brain, constipation, depression, diarrhea, dry mouth, headaches. Hot flashes |
| insomnia, immune suppression, loss of appetite, loss of libido, Lymphedema, mouth sores, | |
| nausea, vomiting, pain, neuropathy, radiation burns, shortness of breath, urinary retention, incontinence | |
| Oncology in TCM | modern disciple, combines classical theory with modern technology and research |
| 腫瘤 Zhongliu | |
| 瘤 Liu (tumor) | |
| 腫 Zhong (swelling) | |
| Accumulation of flow of blood generated a “swollen tumor” Liu Zhong | |
| Modern theory | Cancer (癌 ai) is understood as |
| 正虛邪氣 | |
| zheng xu xie shi • Vacuity of right qi, repletion of pathogenic qi | |
| TCM and Western oncology | Developed over last 5 decades. |
| In China, routine to use both (over 90%). China is heavy on herbal formulas. | |
| In the US, modality of acupuncture is most common in oncology. | |
| Key points: | Cancer is often seen as a local manifestation of underlying constitutional disease. |
| Weaking of resistance in the body, while oncological factor grows. | |
| Goal not necessarily to eliminate cancer, but to increase quality of life. | |
| TCM may suppress cancer growth, promote cancer cell apoptosis, antiangiogensis, and antimetastasis. | |
| May help prevent relapse. | |
| Treatment Continuum | 1. Initial diagnosis |
| 2. As enter and during treatment | |
| 3. Recovery after treatment | |
| 4. Additional rounds of treatment | |
| 5. Transition off-therapy | |
| 6. Surveillance | |
| 7. Long-term recovery to prevent relapse and metastasis | |
| 8. End of Life Care. | |
| Why patients see care. | Reduce stress of illness |
| Improve Quality of Life | |
| Symptom care management | |
| Prevention of late effects | |
| Prevention of second malignancy and relapse | |
| Treatment of Cancer “Try everything possible”. | |
| Key points: | Treatment will combine WM diagnosis and TCM syndrome differentiation. |
| Treatment planning: | patient constitution |
| TCM syndrome | |
| Primary presenting symptoms | |
| Predicted or observable side effects | |
| Anti-neoplastic (anti-cancer attitude) | |
| Shen/mind/mental | |
| Treatment Goals | Mitigate side effects with zero-toxicity treatment |
| Enhance therapeutic effects of chemo and radiation | |
| improve quality of life and long-term survival | |
| Assist patients to better tolerate treatment & complete conventional medical treatment | |
| Restore general health | |
| Modification of integrative care plans | Side effects arise and change |
| Disease progresses and creates new symptoms | |
| Patient progresses through different treatment phases | |
| modality does not bring about desired outcome, requiring different modality or combination | |
| Improvement in symptoms requiring less intervention | |
| Care may shift from patient to family member (s). | |
| syndrome differentiation | Has become an important concept in oncology in China over last decade. |
| is reported by type of cancer | |
| Attempt to understand the molecular basis for each symptom within each cancer to better understand its usefulness in practice | |
| Understanding Cancer in TCM | Stagnation does not always lead to cancer, but it is present in cancer |
| TCM attributes emotions as an important internal disease factor | |
| External causes- lifestyle, exposure, pathogenic factor. | |
| Qi stagnation- fluid accumulation- Blood stasis- Toxin- Cancer? | |
| Blood stasis | very common in cancer patients with liver, lung, and pancreatic cancers. Stabbing pain of cancer |
| Some data suggests increase in metastasis, some not. | |
| Damp Heat | Associated with cancers of the GI tract (Colon, liver, pancreas) |
| Yin vacuity (fluid deficiency) | Commonly seen in cancers of liver, lung, breast, stomach, and colon |
| Spleen Vacuity | Extensive research in China looking at this pattern in cancer |
| Correlation between spleen vacuity and immunological dysfunction | |
| Supplementing the spleen is believed to enhance proliferation of splenic cells and | |
| significantly increase auto-antibody secretory cell number. | |
| Enhance cytotoxic action of lymphocytes. | |
| Fu Zheng | Huang qi (herb) is the cornerstone of the therapy |
| Extensively used as an adjunct to chemotherapy. | |
| Particularly with non-small cell lung cancer with platinum based therapy. | |
| Studies suggest that this increased effectiveness of platinum drugs. | |
| Research suggests longer survival rate. | |
| Zhen Qi Fu zheng Chong Ji | Huang qi- astagalus 20-30g |
| Dang shen/codonopsis 20g | |
| Fu ling/ Poria 10g | |
| Gou qi zi/Lycium fruit 12g | |
| Bu gu zhi/Psoralea fruit 10g | |
| Nu zhen Zi/Ligustrum 12g | |
| Bai Zhu/ atractylodes 12g | |
| Zhi gan cao/ honey fried licorice 6g | |
| Tu si zi/ Cuscuta seeds 12g | |
| Constitutions | Yin vacuity |
| Qi vacuity | |
| yang vacuity | |
| Blood vacuity | |
| Blood heat | |
| Blood dryness | |
| Binding depression of Liver qi | |
| Up flaming of liver fire | |
| Damp heat in LI | |
| Damp heat in UB | |
| Stomach Heat. | |
| Considerations | Assessment and interventions based on clinicians experience-results will differ from clinician to clinician= hard to study |
| Trend is to combine pattern differentiation and disease diagnosis for future cancer TX | |
| Have not determined exact relation between patterns and biological processes. |
| Pain | Subjective component is explicit |
| Included the physiologic sensation and an emotional reaction to that sensation. | |
| Classification of pain | Nociceptive- somatic or visceral |
| Non-Nociceptive- Neuropathic or psychogenic | |
| Neuropathic pain- pain from a lesion or disease of the somatosensory nervous system | |
| Central Neuropathic- central | |
| Peripheral neuropathic pain- peripheral | |
| Neuropathic pain- positive symptoms | Allodynia- pain due to stimulus that does not normally provoke pain |
| Dysesthesia- an unpleasant abnormal sensation, whether spontaneous or provoked. | |
| Hyperalgesia- increased pain from a stimulus that normally provokes pain. | |
| Hyperesthesia- increased sensitivity to stimulation, excluding the special senses | |
| Hyperpathia- syndrome w/abnormal painful reaction to a stimulus, repetitive stimulus, increased threshold. | |
| Paresthesia- abnormal sensation, whether spontaneous or evoked. | |
| Neuropathic pain- negative response | Analgesia= absence of pain in response to stimulation which would normally be painful. |
| Hypoalgesia- diminished pain in response to a normally painful stimulus | |
| Hypoesthesia- decreased sensitivity to stimulation, including special senses. | |
| Negative symptoms: weakness, sensory loss, numbness, light tough, position sense, thermal perception, decreased vibration | |
| Neuropathic pain tissue origin | Cerebropathy ex. Brain tumor |
| Myelopathy- ex. Spine cord compression | |
| Radiculopathy- ex. Ependymoma (spinal cord tumor). Dermatome test.. | |
| Plexopathy- pancost tumor in upper lung radiates down arm | |
| Neuropathy- CIPN (chemo induced neuropathy). Damage/dysfunction of peripheral nerves- motor, sensory and autonomic. | |
| Myotomes | Group of muscles affected by a nerve root. |
| Radiculopathy causes: disk herniation, facet arthropathy, central stenosis, spondylolisthesis | |
| neuropathic pain plexus | Cervical- injury, tumor, radiation, Erb’s palsy (c5-C6), Klumpke’s palsy (C8-T1), TOS, Surgery |
| Brachial- idiopathic brachial plexopathy, neuralgic amyotrophy, brachial neuropathy, brachial neuritis, shoulder-girdle neuritis, etc. | |
| Lumbar | |
| Sacral | |
| Presentation | Chemo: pain, Radiation: paresthesia, weakness |
| Pain | Chemo: early, severe, Radiation: later in course |
| Edema | Chemo: Occasional, Radiation: common |
| Bracial plexus | Chemo: Often lower plexus, Radiation: usually whole plexus |
| Lumbarsacral | Chemo: Lower, usually unilateral, Radiation: commonly bilateral |
| Horner syndrome | Chemo: common, Radiation: Unusual |
| Local tissue necrosis | Chemo: not present, Radiation: common |
| Rectal Mass (LSP) | Chemo: common, Radiation: not a feature |
| Myokymia (EMG) | Chemo: usual, Radiation: may be present |
| Nerve Enhancement (MRI) | Chemo: present, Radiation: usually absent |
| PET Scan | Chemo: positive, Radiation: usually negative |
| Neuropathy causes | Idiopathic, Chemotherapy, Infection, Critical Illness, Toxic, metabolic, compression, inherited. |
| Chemo | Platinum analogues: cisplatin, Carboplatin, Oxaliplatin (affect dorsal root ganglia DNA, sensory neuropathy) |
| Taxanes: Paclitaxel, Abraxane, Docetaxel (tubuline inhibitors, affects long nerves) | |
| Vinca alkaloids: vincristine, vinblastine, vinorelbine, vindesine (affects long nerves) | |
| other: Bortezomib, Ixabepilone, thalidomide, Lenalidomide. (blood supply issues) | |
| Etiology of neuropathy | Direct effect: nerve infiltration or compression |
| Paraneoplastic effect: remote effect of antibody, hormone, protein | |
| Iatrogenic effect: chemotherapy, radiation, Immunosuppression, Graft vs host disease. | |
| Distribution | Polyneuropathy |
| Mononeuropathy | |
| Mononeuropathy multiplex | |
| Ganglionopathy | |
| Small fiber Neuropathy | |
| Autonomic Neuropathy | |
| Nociceptive pain | pain arising from actual or threatened damage to non-neural tissue and is due to the activation of nociceptors. |
| pathophysiology | activation of nociceptors (A delts or C fibers0 by noxious stimuli that can be mechanical, thermal, or chemical. |
| Nociceptors may be sensitized by endogenous chemical stimuli such as serotonin substance P, bradykinin, prostaglandin, histamine. | |
| Generally described as dull or achy, exacerbated by movement and relieved with rest, localized, and reproducible. | |
| Nociceptive pain can hurt on touch while neuropathic will not. | |
| examples: | rotator cuff tendonitis, adhesive capsulitis, epicondylitis, De Quervains Tenosynovitis, spinal stenosis, spinal instability, fracture |
| arthritis, enthesopathy, GVHD, Scoliosis. | |
| Upper pain disorders in Breast Cancer | neuromuscular: cervical radiculopathy, brachial plexopathy, polyneuropathy, mononeuropathy, post mastectomy pain |
| lymphovascular: lymphedema, axillary web syndrome, post thrombotic syndrome | |
| Musculoskeletal: post surgy pain, rotator cuff disease, bicipital tendonitis, adhesive capsulitis, bony metastases, deQuervains, arthritis | |
| integumentary- cellulitis, radiation dermatitis | |
| Treatment modalities | Non-pharmacological- exercise, weight loss, PT, Otm lymphedema education |
| Pharmalogical- anti-inflammatories, nerve stabilizers, analgesics | |
| Surgical- laminectomy, injections, nerve block | |
| Pain management | Patient education, weight loss, PT, Ot, assistive devices (cane, neck collar), Orthotics, Modalities |
| posture training. | |
| Pt: Neuromuscular re-education- postural, PNR proprioceptive neuromuscular re-education, core strengthening, scapular retraction, | |
| Muscle balancing, Soft tisue mobiliztion like Myofacial release, visceral therapy, Craniosacral therpay, MLD | |
| non-pharmacological therapy | heat, cold, electrotherapy, laser, reduce pain, aid wound healing, facilitate tissue compliance, introduce medication, corticosteroid |
| superfical heat | heat pads, moist compress, hydrocollator packs, paraffin bath, whirlpool bath |
| contraindication: acute trauma, bleeding, edema, vascualr disease, large scars, impaired sensation, cognitive deficits. | |
| Deep heating | to muscles, tendons, bones, like ultrasound, mosit heat, laser, TENs, avoid in tumor areas. |
| Cryotherapy | pain and inflammation musculoskeletal disorders, myofascial pain, spasticity, minor burns. |
| contra: cold hypersensitivity, raynaud’s | |
| Pharmacological | opioids (morphine, methadone, oxycodone, NSAID, corticosteroid, |
| Nerve stabilizers: anticonvulsants, Tricyclic antidepressants, Serotonin norepinephirine reuptake inhibitors (cymbalta) | |
| Muscle relaxants, | |
| injuctions: corticosteroid, Lidocaine, botox | |
| Topical: capsaicin, lidocaine | |
| Other: tramadol, NMDA antagonists, clonidine | |
| Tramadol- weak synthetic analogue of codeine, 1/10 of morphine | |
| Seratonin norepinephirine reuptake inhibitors (cymbalta)- caution with Tamoxifen. Side effcts: nausea vomit,consipation, dirrhea | |
| Gabapentin (Neurontin) and Pregabalin (Lyrica)- dizziness, somnolence, weight gain, withdrawl | |
| Non-specifi NSAIDs: aspirin, ibuprofen, naproxen, diclofenac, celebrex, vioxx. Side effects: Cardio risk, GI risk | |
| Conclusion | Neuropathic, somatic, and mixed pain disorders should be carefully diffferentiated using history, physicla exam, imaging, and |
| diagnostic testing where appropriate. | |
| Treatment modalities should be chosen based on an accurate assessment of the patients pain so as to have | |
| maximal efficacy while minimizing adverse events. | |
| multimodal pain management is often needed to achieve optimal outcomes. |
| Psychiatric and Psychological | |
| Depression in cancer patients | 3 to 58%, the majority falls in the 10 to 25% |
| Depression if 4x greater in cancer than general population | |
| More prevalent in advanced cancer like pancreatic 40-50% | |
| Children with cancer 10-14% | |
| associated with increase in morbidity and impacts negatively on survival. | |
| Diagnostic assessment | DMS. Gold standard Diagnostic and statistical manual. |
| Endicott substitution criteria | |
| Research diagnostic Criteria | |
| Structured diagnostic interviews | |
| Schedule for affective disorders and schizophrenia | |
| Diagnostic interview schedule | |
| Structured clinical interview for DSM-III-R | |
| Screen instruments self-report: | |
| General health questionnaire | |
| Hospital anxiety and depression scale | |
| Beck depression inventory | |
| Depression | Persistent, prominent, dysphoric mood, loss of interest in most activities |
| Somatic sx: insomnia, hypersomnia, weight or appetite change, fatigue, psychomotor agitation | |
| Psychological sx: feeling worthless, suicidal thoughts, memory and concentration difficulties. | |
| Approaches | Inclusive approach- includes that cancer treatment comes with depression symptoms and treat with anti-depressant. |
| Exclusive approach- may miss that patient is depressed and not treat them. | |
| Etiologic Approach- from cancer, illness, or depression. | |
| Substitutive approach- depressed appearance, social withdrawal, decreased talkative, brooding, self-pity, pessimism. | |
| Increased Threshold Approach- 7 symptoms | |
| Brief screening: “have you been depressed most of the time for the past two weeks?” two-item interview, visual analog, Beck inventory | |
| Medical conditions depression | Uncontrolled Pain |
| Metabolic abnormalities like Hypercalcemia, sodium or potassium imbalance, Anemia, Def. B12 or folate. | |
| Endocrinologic Abnormalities: Hyper- Hypothyroidism, Adrenal insufficiency. Low T in men. | |
| Medications can affect neurotransmitters causing symptoms. | |
| Steroids, Interferon (renal, melanoma) and interleukin 2, Methyldopa, Reserpine, Barbiturates, Propranolol, | |
| Chemo agents: Vincristine (All, brain), Vinblastine (breast and Lung cancer), Procarbazine (Brain), L-Asparaginase. | |
| Corticosteroids in Lymphoma patients, antibiotics (amphotericin B), Tamoxifen (Breast), Cyproterone (Prostate). | |
| Cytokines (pro-inflammatory) | depressed mood, dysphoria, anhedonia, helplessness, fatigue, weight loss, hypersomnia, psychomotor retardation, confusion, |
| lack of concentration, anorexia. Cytokines- CNS and the brain affected. | |
| IL-1, IL-6, TNF-alpha cytokines. Anti-depressants can help. | |
| Depression other: | Depression and hastened death (like AIDS patients) with anti-depressant the desire to die decreased. |
| Tricyclic antidepressants low dose 25-125. Duloxetine was found to be very effective. | |
| Antidepressants that can affect Tamoxifen chemo: Venlafaxine, Mirtazapine, Bupropion, Escitalopram. | |
| Psychostimulants | Quicker acting anti-depressants: dextroamphetamine, methylphenidate, modafinil, Pemoline (removed due to liver toxicity) |
| Mood, energy, cognition, improved. Fatigue and appetite improved. | |
| Delirium in Cancer patients | 15-305 in hospitalized patients, 40-80% in advanced disease, palliative care. |
| Harm to self, family, staff, mortality. Interferes with symptom assessment and control. | |
| Untreated can result in dementia or cognitive disorders | |
| pathophysiology of delirium- supports the role of psychopharmacologic management, dopamine blockers. | |
| assessment | DSM |
| Delerium symptom interview | |
| Confusion Assessment method | |
| Delerium rating scale, confusion rating scale, memorial delirium assessment scale | |
| cognitive impairment screening scale: mini-mental state exam, Short portable mental status Questionnaire, cognitive capacity screening | |
| Criteria | Disturbance of consciousness, awareness of environment, reduced focus, shifting attention. |
| change in cognition- memory deficit, disorientation, language disturbance, perceptual disturbance. | |
| Evolve over a short period of time, fluctuate throughout the day. Medical condition etiologically related to disturbance. | |
| Delirium is a disturbance of arousal and cognition. Subtypes: hyperactive (24%), hypoactive, mixed (36%). | |
| Hypoactive delirium is under diagnosed. These patients are quiet, appear depressed, and less distress and delusions. 48% | |
| Tx: antipsychotics. Prevent and reverse etiology, control symptomatology. | |
| Delirium in advanced cancer | Direct: primary brain tumor, metastatic spread |
| Indirect: hypoxia, Metabolic encephalopathy, electrolyte imbalance, withdrawal states. | |
| other causes: | Chemo agents, steroids, radiation, opioids, anticholinergics, antiemetics, infection, |
| Hematologic abnormalities, nutritional deficiencies, paraneoplastic syndromes. | |
| non-pharmacological therapy | Minimize use of catheters, IV lines, physical restraint, monitor for dehydration and electrolyte, nutrition, control pain |
| Minimize medications, sleep hygiene, re-orient frequently. | |
| Pharmacological prevention of delirium has mixed results, they do not prevent delirium in palliative care setting. | |
| Dexmedetomidine use as anesthetic may lower post-op delirium significantly. | |
| Haloperidol < 4.5 mg and (atypical antipsychotics like olanzapine and Risperdal) are effective in managing symptoms. | |
| Risk of stroke, death using these drugs. |
| Palliative Care for pain and symptoms | specialized medical care for people living with serious illnesses. It focuses on providing relief from the symptoms |
| and stress of serious illness. It is appropriate at any age and stage of a serious illness and provided along with curative treatment. | |
| palliative is | Evidence based medicine (EBM), provided alongside efforts to cure an illness, good at pain and symptom management |
| through the illness, patients and family centered, focuses on quality of life as defined by the patient and family unit. | |
| Palliative care is not | giving up on a patient, in place of curative or life-prolonging care, limited to specialists, same as hospice. |
| Hospice | compassionate care at the end of life, team-oriented to expert medical care and pain managment, emotional and spiritual support. |
| Provided in a variety of settings including home, resident facility, hospitals, etc. | |
| Medicare hospice benefits is provided to those who have been medically certified as terminally ill with a prognosis <6 months to live. | |
| Old model | diagnosis- disease modifying treatment- terminal phase of illness-palliative care- hospice. |
| current care continuum | diagnosis- disease modifying treatments-palliative care- terminal phase of illness-. Hospice- death-bereavement. |
| QOL – quality of life, EOL- end of life | |
| Importance of Palliative Care: | goals and needs change. Patients go through many stages of illness, personhood, life relationships, perspectives, QOL |
| better outcomes for patients, family, providers: focus on symptoms and pains through treatments not just EOL. | |
| Explore worries, fears, hope throughout the treatment. | |
| assess patient and family needs | |
| improve our communication on multiple levels. | |
| Healthcare utilization | |
| Life expectancy | 1900- 47yo. 2000- 75yo. |
| Usual place of death | 1900- Home, 2000- Hospital. |
| Reason for Death | 1900- Infectious disease, communicable disease. 2000- Chronic illness. |
| Most medical Expense | 1900- Paid by family, 2000- paid by Medicare. |
| Disability before Death | 1900- Not common, 2000- average of 2 years. |
| Integration of Palliative Care | study found palliative care has meaningful improvements in QOL and mood, patient was less depressed, the patient received less |
| aggressive care as they got sicker, increased advance directives and DNR wishes documented, average life | |
| expectancy was ~3 months longer than those who received usual oncological care alone. | |
| Palliative Care Team | Doctors, nurses, specialists working with other doctors to provide an extra layer of support. |
| MD’s, Nurse practitioners, Office practice nurses, social workers, pharmacists, | |
| Chaplain, Integrative practitioner, Medical and Nurse fellows. | |
| Reason to consult | pain and symptom management |
| complex psychosocial/spirit support required | |
| assistance in clarifying goals of care | |
| assistance in withdrawal of life sustaining treatment | |
| Actively dying patient requires specialist input | |
| complex disposition planning. | |
| Palliative Care assessment | Review clinical course |
| Focused assessment of chief complaint | |
| Disease understanding | |
| dignity therapy question | |
| Brief symptom assessment scale | |
| Detailed social history | |
| Spiritual assessment | |
| patient and family goals of care | |
| Pharmacologic and non-pharmacologic care, holistic treatment | |
| Cancer Symptoms | Pain, vomit, nausea, fatigue, Insomnia, Anorexia, Dyspnea, anxiety, depression, distress. |
| complementary and integrative therapy | reduced therapy related toxicity, improvement in disease-related symptoms, improve QOL |
| pain management | Pain is an unpleasant sensation and emotional experience associated with actual or potential tissue damage. |
| whatever a person experiencing it says it is. Exisiting where the person says it does. | |
| Physiologic sensation and emotional reaction to that sensation= total pain. | |
| Cancer and pain | cancer patients experience pain throught treatment |
| 1/3 actively receiving cancer treatment | |
| 2/3 of persons with advanced malignancy | |
| 3/4 of persons with advanced cancer admitted to the hospital experience pain on admission | |
| 54% of patients near the end of life. | |
| Causes | 60-65% tumor invasion in metastatic disease |
| 20-25% treatment related pain to surgery, chemo and radiation | |
| 10-15% chronic conditions | |
| pain vs suffering at end of life | Existential distress, uncertainty of illness, loss of control |
| dimensions of QOL, requires interdisciplinary assessment and management. | |
| Guidelines of pain management | Interdisciplinary approach, cultural considerations, assessment should be regular and on-going, |
| for controlled substances implement a risk management plan, document response, educate family, | |
| identify and address barriers, address suffering, refer to providers with specialized skill. | |
| Assessment of pain (OLDCART) | Onset, Location, duration, characteristics, aggravating factors, Relieving factors, therapies tried |
| patient description of pain | |
| meaning of pain | |
| how pain impacts quality of life (QOL) | |
| Cultural considerations | |
| Goals of care | |
| medication use history: current, past, what worked, what didn’t? | |
| psychosocial history: family friend support, substance use history? | |
| Pharmacological mgmt of pain | Non-opioids: acetaminophen, analgesic/antipyretic, NSAID- antipyretic, anti-inflammatory, analgesic. Adverse effects. |
| Opioids- morphine, oxycodone, oxymorphone, fentanyl, hydromorphone, metadone. | |
| less common- Buprenorphine, codeine, hydrocodone, tapentadol, tramadol. Adverse: respiratory depression, constipation, sedation. | |
| Adjuvants analgesics: anticonvulsants for neuropathic nerve pain: gabapentin and pregabalin | |
| anti-depressants: tricyclic serotonin-norepinephrine reuptake inhibitors (SNRIs) | |
| local analgesics- topical, intravenous, spinal. | |
| Corticosteroids- activates/increase appetite, side effect with prolonged use. | |
| Routes | oral, transmucosal, rectal, transdermal, topical, parenteral, spinal. |
| Interventional therapies | neurolytic blocks |
| neuroblative procedures | |
| vertebroplasty/kyphoplasty | |
| epidural steroid injection | |
| Intrathecal pump | |
| Non-pharmacologic strategies | Physical: rehab medicine, exercise, cold/heat, self-care, walking. |
| Psychosocial: CBT, psychotherapy, relaxation, meditation, hypnosis, music therapy | |
| Complementary/Integrative: systemic desensitization. Acupuncture/acupressure, Yoga, Tai Chi, massage, Reiki, Qigong. | |
| Conclusion | Palliative care focuses on providing relief from the symptoms and stress of serious illness at any stage. |
| It is not the same as Hospice care. The approach to pain is interdisciplinary. | |
| Acupuncturists play a vital role in symptom management and support. Pain relief is necessary and highly achievable. | |
| Acupuncture mechanisms of Action | Biomed mechanism of actions for acupuncture |
| Fascia and connective tissue | |
| Neurotransmitters and the autonomic nervous system | |
| Neuro-imaging studies | |
| Conveying the information to other health care professionals. | |
| Objectives | List neurotransmitters involved in analgesic effect of acupuncture |
| Describe evidence of modulation of ANS by acupuncture | |
| Summarize finding in neuro-imaging of acupuncture | |
| Explain the current evidence of mechanisms of action for acupuncture to health care professionals. | |
| Acupuncture Consensus | Acupuncture is becoming more accepted n an Oncology setting for pain and symptom management |
| Data shows measurable neurological effects | |
| Clearly communicating mechanisms of action to the medical team will improve understanding and benefit patient care. | |
| Acupuncture points and myofascia | location of acu points and meridians in a serial gross anatomical sections through a human arm. |
| Ultrasound and de qi- twisting cause changes in collagen fibers. Nervous sensors on myofascial planes, cause downstream events. | |
| How it works? | TCM- theraputic effect results from manipulation of flow of qi in meridian. This is too unfamiliar with western health care pros. |
| Neuroscience research helps with neuroanatomy and physicology to help explain to western health care professionals. | |
| Endogenous Opioids | Acupuncture helps stimulate the discharge of endogenous (internally sourced) opioids- substances that suppress pain. |
| This discovery initiated a scientific and evidence based explanation for the mechanism of acupuncture. | |
| Stimulation of the acupoint by a needle sets off a nerve signal to the brain to release endorphins, | |
| acupuncture may activate additional neural pathways and neurotransmitters. | |
| Endomorphin-1, beta endorphin, enkephalin, and serotonin levels in plasma and brain tissue. | |
| Analgesia by acupuncture | Is blocked by opioid receptors blockers. Tolerance to pain. |
| E-acupuncture: analgesia Yes | |
| E-acupuncture and Saline: analgesia Yes | |
| E-acupuncture and naloxone: analgesia No | |
| Sham E-acupuncture at non-acupoint: analgesia No | |
| Saline alone: analgesia No | |
| Naloxone alone: analgesia No | |
| No treatment: analgesia No | |
| Different receptors at diff locations | 2 hz and 15 hz: two opioid receptors |
| 100 Hz: another different opioid receptor | |
| local injection of antibodies or chemical | 2 hz- neurotransmitter B-endorphins location in midbrain |
| (old study) | 2 hz- Enkephalins in the spinal cord |
| 100 Hz- Dynorphins in the spinal cord | |
| New study- Adenosine | Adenosine peaking up to 200 microdialysate(nm) in 30 minutes |
| AMP peaking up to 400 in 30 minutes. | |
| Pain pathway: | trauma to skin- peripheral nociceptors engage- local anesthestics and anti-inflammatory drugs |
| local anesthetics to peripheral n. | |
| dorsal ganglion root- to the dorsal horn (local anestheris, opioids, alpha2agonists) of spinal cord- up spinothalamix tract to brain. | |
| pain- perceived by brain (opioids, Alpha2agonists)- descending modulation back to dorsal horn. | |
| Acupuncture gives additional signs around this pathway, suppress the conduction of pain signals up to the brain. | |
| Yin and yang: autonomic N. system | Sympathetic is like Yang: hot, breathing changes, dilation, excitement, fight and flight. |
| Parasympathetic is like Yin: quiet, relaxing, HT rate down, digest and rest. | |
| LI4 regulates Sympathetic N.S. 2 hz and 20 hz. , low frequency increases parasymathetic, tonic. 20 hz phasic- comes and goes. | |
| St36 on digestion: digestive tract movement, 10 min. e-stim promoted the GI tract to move for up to 2 hours. | |
| Hypertension and BP | e-stim inhibition of cardiovascular sympathetic neurons that have been activated through visceral reflex stimulation. |
| this is mediated through activation of neurons in the arcute necleus of the hypothalamus, vLPAG in the midbrain, and NRP in medulla. | |
| Glutamate, acetylcholine, opioids, GABA, nociceptin, serotonin, and endo-cannabinoids all appear to participate in the E-stim | |
| hypotensive respnse although their importance vararies between nuclei. | |
| Acupuncture and neuroimaging studies | MRI- activation and deactivation of cortical regions using LI2. Saliva production also increased. |
| theory- stimulated the parasympathetic ns to produce more saliva. | |
| parts of brain light in in MRI with acupuncture. Body and somatic signals. | |
| Acupuncture and Limbic system | Limbic is part of regulation of moods, emotions like fear, anger, anxiety. |
| responder’s vs non-responders when getting acupuncture. Some people do not seem to respond to acupuncture. | |
| Summary | Still much is unknown how acupuncture works, strong evidence is coming from neuroscience. |
| Clinically it is found acupuncture can modulate the nervous system at the molecular level (neurotransmitters), and matrix | |
| level like activating or deactivating certain neural circuits. |
| Acupuncture mechanisms of Action | Biomed mechanism of actions for acupuncture |
| Fascia and connective tissue | |
| Neurotransmitters and the autonomic nervous system | |
| Neuro-imaging studies | |
| Conveying the information to other health care professionals. | |
| Objectives | List neurotransmitters involved in analgesic effect of acupuncture |
| Describe evidence of modulation of ANS by acupuncture | |
| Summarize finding in neuro-imaging of acupuncture | |
| Explain the current evidence of mechanisms of action for acupuncture to health care professionals. | |
| Acupuncture Consensus | Acupuncture is becoming more accepted n an Oncology setting for pain and symptom management |
| Data shows measurable neurological effects | |
| Clearly communicating mechanisms of action to the medical team will improve understanding and benefit patient care. | |
| Acupuncture points and myofascia | location of acu points and meridians in a serial gross anatomical sections through a human arm. |
| Ultrasound and de qi- twisting cause changes in collagen fibers. Nervous sensors on myofascial planes, cause downstream events. | |
| How it works? | TCM- theraputic effect results from manipulation of flow of qi in meridian. This is too unfamiliar with western health care pros. |
| Neuroscience research helps with neuroanatomy and physicology to help explain to western health care professionals. | |
| Endogenous Opioids | Acupuncture helps stimulate the discharge of endogenous (internally sourced) opioids- substances that suppress pain. |
| This discovery initiated a scientific and evidence based explanation for the mechanism of acupuncture. | |
| Stimulation of the acupoint by a needle sets off a nerve signal to the brain to release endorphins, | |
| acupuncture may activate additional neural pathways and neurotransmitters. | |
| Endomorphin-1, beta endorphin, enkephalin, and serotonin levels in plasma and brain tissue. | |
| Analgesia by acupuncture | Is blocked by opioid receptors blockers. Tolerance to pain. |
| E-acupuncture: analgesia Yes | |
| E-acupuncture and Saline: analgesia Yes | |
| E-acupuncture and naloxone: analgesia No | |
| Sham E-acupuncture at non-acupoint: analgesia No | |
| Saline alone: analgesia No | |
| Naloxone alone: analgesia No | |
| No treatment: analgesia No | |
| Different receptors at diff locations | 2 hz and 15 hz: two opioid receptors |
| 100 Hz: another different opioid receptor | |
| local injection of antibodies or chemical | 2 hz- neurotransmitter B-endorphins location in midbrain |
| (old study) | 2 hz- Enkephalins in the spinal cord |
| 100 Hz- Dynorphins in the spinal cord | |
| New study- Adenosine | Adenosine peaking up to 200 microdialysate(nm) in 30 minutes |
| AMP peaking up to 400 in 30 minutes. | |
| Pain pathway: | trauma to skin- peripheral nociceptors engage- local anesthestics and anti-inflammatory drugs |
| local anesthetics to peripheral n. | |
| dorsal ganglion root- to the dorsal horn (local anestheris, opioids, alpha2agonists) of spinal cord- up spinothalamix tract to brain. | |
| pain- perceived by brain (opioids, Alpha2agonists)- descending modulation back to dorsal horn. | |
| Acupuncture gives additional signs around this pathway, suppress the conduction of pain signals up to the brain. | |
| Yin and yang: autonomic N. system | Sympathetic is like Yang: hot, breathing changes, dilation, excitement, fight and flight. |
| Parasympathetic is like Yin: quiet, relaxing, HT rate down, digest and rest. | |
| LI4 regulates Sympathetic N.S. 2 hz and 20 hz. , low frequency increases parasymathetic, tonic. 20 hz phasic- comes and goes. | |
| St36 on digestion: digestive tract movement, 10 min. e-stim promoted the GI tract to move for up to 2 hours. | |
| Hypertension and BP | e-stim inhibition of cardiovascular sympathetic neurons that have been activated through visceral reflex stimulation. |
| this is mediated through activation of neurons in the arcute necleus of the hypothalamus, vLPAG in the midbrain, and NRP in medulla. | |
| Glutamate, acetylcholine, opioids, GABA, nociceptin, serotonin, and endo-cannabinoids all appear to participate in the E-stim | |
| hypotensive respnse although their importance vararies between nuclei. | |
| Acupuncture and neuroimaging studies | MRI- activation and deactivation of cortical regions using LI2. Saliva production also increased. |
| theory- stimulated the parasympathetic ns to produce more saliva. | |
| parts of brain light in in MRI with acupuncture. Body and somatic signals. | |
| Acupuncture and Limbic system | Limbic is part of regulation of moods, emotions like fear, anger, anxiety. |
| responder’s vs non-responders when getting acupuncture. Some people do not seem to respond to acupuncture. | |
| Summary | Still much is unknown how acupuncture works, strong evidence is coming from neuroscience. |
| Clinically it is found acupuncture can modulate the nervous system at the molecular level (neurotransmitters), and matrix | |
| level like activating or deactivating certain neural circuits. |
| Acupuncture for cancer pain | Science and Cancer pain, evidence on Oncology acupuncture for pain, research on oncology acupuncture for pain. |
| 53% of all cancer patients will have pain, 33% cancer surviors after cureative treatment, 59% patients undergoing cancer treatment, and | |
| 64% in advanced metastatic or terminal cancer.- van den Beuken Everdingen et al. (Prevelence of cancer pain) | |
| Cancer is complex | through all stages: active tx, palliative care, survior-ship. |
| mult-factored: disease, psycho-social, treatment. | |
| Treatment: surgery, chemo, radiation, Targeted Tx, hormonal tx, Immune tx. | |
| Nociceptive pain: 1) somatic like arthritis pain, 2) visceral like ascities causing abdominal pain | |
| Neuropathic pain: ex. Neuropathy (from chemo) | |
| Common pain medications: | Opioids (long: Oxycontin, fentanyl patch | Short: Percocet, Dilaudid) |
| Anticonvulsants (Gabapentin, Pregablin), | |
| Antidepressants (Duloxetine), | |
| NSAIDS (Motrin, Naproxen) from mild muscular skeletal | |
| Acetaminophen.(prolonged use can cause liver damage. | |
| Mechanisms of Acupuncture | Stimulation of acupuncture sites releases endogenous opioids in brain. |
| Opioid antagonists block analgesic effects of acupuncture | |
| electric acupunctre/e-stim/EA: | 2 Hz: b-endorphins, endomorphin, enkephalin, targeting new and delta receptors.Brain releases these. |
| 100 Hz: dynorphin, targeting k receptor. Spine releases these. | |
| fMRI brain scans: meta analysis 779 papers identified. 34 eligible for meta-analysis. | |
| Brain response to acupuncture stimuli encompasses a broad network of regions consistent with not just somatosensory, but also | |
| affective and congnitive processing. While results are heterogeneous, from a descriptive perspective most studies suggest that | |
| acupuncture can modulate the activity within specific brain areas, and the evidence based on meta-analysis confirms some of | |
| these results. More higher quality studies with more transparent methodology are needed to improve the consistency | |
| amoung different studies. | |
| Limbic system- congnition and emotion. Psychological aspects of pain both acute and chronic. | |
| Randomized Controlled Trials (RCT) review 15 RCTs. Acupuncture was not better than drug Tx (n=886, RR: 1.12, P= .09) | |
| However combination of drug treatment and acupuncture was significantly better (n=437, RR: 1.36, P= .003). | |
| Limitations: high risk of bias, substantial methodological limitations. | |
| Conclusion: could not be drawn, future rigourous RCTs necessary to assess clinical efficacy of AC for cancer pain. | |
| Interventions | pts educated on joint pain, told to stay active and continue with usual medical care. |
| electro-acupuncture: 2x week for 2 weeks and 6 weekly after. Manualized protocol “Bi syndrome” patients, | |
| add points for constitution, fatigue, anxiety. 2 Hz at points localized joint pain. | |
| primary- joint pain, brief pain inventory (BPI) | |
| secondary- fatigue, sleep, anxiety, depression | |
| 30% in pain reduction with electro acupuncture vs Sham acupuncture in baseline expectancy. | |
| Responders vs non-responders to acupuncture exist. People who believe acupuncture works, even sham acupuncture worked on them. | |
| Mind-Body effects of acupuncture: a patient feels some relief and begins to feel acupuncture is working. | |
| Sham acupuncture- you expect it to work and so it does (top down approach). | |
| high expectation patient need light treatment, low expectation patients needs E-stim acupuncture. | |
| Process acupuncture: art and science | 50%: 1) diagnosis, 2) patient care, 3) patient rest 4) psycho-social support. |
| 50%: the treatment using needles, tui-na, Moxa, guasha, herbs, etc. | |
| note: Acupuncture can produce analgesia (loss of pain sensation) , but effects of acupuncture were blocked by opioid antagonists. | |
| Oncology acupuncture:CINV | Most common symptom, more common in chemo than radiation. Acute, delayed (after chemo), anticipatory (psychological). |
| some can be medical emergencies. | |
| Medical emergencies | Increased intercranial pressure: brain mets/swelling/bleeding. Headache with projectile vomiting. |
| Seen in brain tumor or cancer that spreads to brain like lung, breast, melanoma, etc. | |
| Bowel obstruction: from inside (stomach/colon/rectal cancer) or outside (GYN/peritoneal/sarcoma) obsturction | |
| usually has abdomnal bloating/pain and reduced bowle movement | |
| Systemic illness (serious infection, heart attack, metabolic disorders, etc.) | |
| emetogenic chemo drugs | High: cisplatin, cyclophosphamide, dacarbazine, combo of drugs |
| Moderate: Bendamustine, Carbo/Oxali-platin, cyclophosphamide, cytarabine, Dauno/epi/doxo-rubicin, Ifosfamide, Irinotecan. | |
| Low/Minimal: wide list, but not a severe as above. | |
| Acute emesis meds | One, two or three: |
| 5-HT3 receptor antagonists: Ondasetron (zofran), palonosetron (Aloxi), side: constipation/headache | |
| Neurokinin-1 receptor antagonists: aprepitant (emend), Rolapitant (Varubi), side: fatigue, hiccup | |
| Glucocorticoids: dexamethosone (decadron), side: insomnia, hyperglycemia | |
| Acupuncture | Established cause and primary doctor is aware of. |
| If significant and worsening, communicate with primary doctor. | |
| other situation | Delayed from chemo: Olazapine or metoclopramide |
| Anticipatory- relaxation, hypnosis, ginger, lorazepam (Ativan) | |
| Difficult to control- consider cannabinoids/medical marijuana. | |
| Patient assessment | Anti-nausea meds not working well, minimal relief, wants less meds, acupuncture for other things as well as nausea. |
| Chemo schedule, onset of symptoms, corticosteroids may delay symptoms, check labs: contraindicatins: ANC < 0.5 , platelets < 20k. | |
| Treatment planning | Prior to chemo, when symptoms appear, sever: 2x per week, during episode 10 hz, 25 minutes. |
| special considerations: difficulty lying prone or supine, enusre they can reach you/call button, have bucket close. | |
| Tx strategy: chemo/radiation is a toxic heat, principle: clear heat, harmonzie center, fortify ST/SP. | |
| Common patterns | SP damp (bloating, swelling, const./diarrhea), ST heat (reflux, red), KD vacuity (wasting, diarrhea, SOB) |
| Point Prescription | Pc6, LI11, ST36. SP damp: pc6, ren12, st36, Sp9, ST heat: PC6, Li11, St25, St44, KD vacuity: PC6, ST36, KD3, Du20 |
| acute episode: pc6, st36, in between episode- support ST/SP, clear heat, harmonize center.moxa/TDP. | |
| Additional Tools | teach acupressure PC6, seasickness bands, ear seeds (shenmen), mind-body imagery/meditatin, ginger, peppermint, moderate exercise. |
| Chemo induced Peripheral neuropathy | (CIPN) |
| CIPN common adverse effect from certain treatments: Taxanes, platinum, vinca alkaloids, bortezomib, and thalidomide | |
| sx: pain, numbness, tingling, weakness, autonomic neuropathy (incontinence, bowel movement). | |
| Long-term effects on quality of life and can continue for years. | |
| Taxanes- breast and ovarian cancer patients. Axonal microtubule structure disruption. | |
| Platinums- colo-rectal, sometimes ovarian patients. Dorsal root ganglia damage, mitochondrial dysfunction, neural apoptosis, | |
| either by DNA crosslinking or oxidative stress. | |
| Vinca alkaloids- liquid tumors like lymphoma. Alterations in neuronal cytoskeleton causing axonal degeneration. | |
| Bortezomib-multiple myeloma | |
| Thalidomide- multiple myeloma | |
| 48% of cancer patients have CIPN, 61% in first month of chemo, 30% after 6 months of completing chemo. | |
| Unpredictable course | many improve, or persist, or worse over time du to permanent damage to nerves. |
| 6 years symptoms can persist for breast and colon cancer patients. | |
| risk factors | Baseline neuropathy, diabetes, Smoking, decreased creatine clearing, pharmocogenomics. |
| Assessment CIPN | Objective: Neurological, vibration sensation test, nerve conduction |
| Subjective: NCI-CTCAE, patient reported outcomes, composite scales: TNS | |
| Reduction of chemo may be done to help with CIPN. | |
| RCT: E-stim acupuncture actually made CIPN worse and Sham Acu was better result. | |
| Nervous system disorder | |
| Peripheral motor neuropathy | grade 1: asymptomatic, clinic or diagnostic observation only, intervention not indicated |
| grade 2: moderate symptoms, limiting instrumental ADL | |
| grade 3: Severe symptoms, limiting self care ADL, assistive device indicated. | |
| grade 4: Life threating consequences, urgent intervention indicated | |
| grade 5: death | |
| Peripheral sensory neuropathy | grade 1: Asymptomatic, loss of deep tendon reflexes or paresthesia |
| grade 2: Moderate symptoms, limiting instrumental ADL. | |
| grade 3: Severe symptoms, limiting self care ADL | |
| grade 4: Life threating consequences, urgent intervention indicated | |
| grade 5: death | |
| positive trial: Duloxetine | |
| There are studies that show acupuncture may be effective in persistent CIPN, however is not a cure for nerve conduction damage. | |
| CIPN presentations | tingling, numbness, burning sensation, pain, cramping, muscle weakness, sensitive to heat or cold or touch |
| balance issues, altered gait. | |
| may develop weeks or months after chemo, starting in fingers and toes then progress towards the body | |
| CIPN may result in limiting, delaying, or discontinuing chemo. Gabapentin and pregabalin may be used in treatment, not a cure. | |
| Acupuncture | increase blood flow to limbs, improver sensory/motor n. conduction, accelerating nerve repair, decrease neuropathic pain |
| early intervention and frequency treatments may increase efficacy. | |
| Caution: lymphedema or local infection. | |
| Patterns CIPN | toxins invading channels, qi and blood stagnation, qi and blood deficiency, Internal wind, Damp accumulation. |
| acu: Li4, Li11, TB5, ST36, GB34, Liv3, Bafeng (feet), and Baxie (hands) | |
| sp6 and liv8 for blood deficiency | |
| sp9/st40 for phelgm | |
| Li11 and Liv2- clear heat | |
| retain needles 30 min. 2-5 hz , pulsing sensation, pacemaker (estim contraindicated) | |
| 1x for 10 weeks. Severe” 2x a week. | |
| Other: massage therapy, reflexology, physical therapy, exercise | |
| Acupuncture is helpful in reducing CIPN symptoms. | |
| Cancer Related Fatigue (CRF) | CRF- distressing, persistent, subjective, physical, emotional, cognitive tiredness, exhaustion, interferes with usual functioning. |
| Epidmiology | between 9-90% prevalence according to diagnostic criteria. |
| 1/3 to 1/4 will have fatigue beyond treatment | |
| High during chemo and radiation, in advanced disease and bone metastasis. | |
| Consider contributory factors: | sleep quality, metabolism, emotional health/mood disorders, medication adverse effect |
| Cardiovascular/Respiratory/oxygen, pain | |
| Anemia, CHF, hypo/hyper thyroid, medications, depression. | |
| CRF | Low clinical priority, no definitive diagnostic work up, no definitive treatment, patient feels dismissed. |
| There are proven behavioral and non-pharmacologic interventions | |
| ICD-10 | Sx present every day during 2-week period in the past month. |
| significant fatigue, diminished energy, increased need to rest, disproportionate to recent change in activity. | |
| 5 of these: general weakness, limb heaviness | |
| diminished concentration or attention, decreased motivation, | |
| insomnia, hypersomnia, | |
| sleep unrefreshing, struggle to overcome inactivity | |
| emotional to feeling fatigue | |
| Difficulty to completing daily tasks, short term memory issues, fatigue lasting hours. | |
| Measure of Fatigue | 0-10, 0-3 none/mild, 4-6 moderate, 7-10 severe. |
| Timing and impairment. | |
| General strategie for fatigue | self-monitor fatigue levels, prioritize energy conservation, pace, delegate, schedule activities |
| use labor saving devices, postpone nonessential activities, limit naps, structure daily activity, one activity at a time | |
| find meaning in current situation, | |
| Nonpharmacy: | exercise program based on limitations (degree of stage of cancer), walk, job, swim, yoga, tai chi, massage, CBT, |
| nutritional support , CBT for sleep, sleep hygiene. MBSR and acupuncture. | |
| Fatigue during active treatment | cyclical and self-limiting, delayed onset of symptoms, symptoms may resolve during the intervals |
| Mild and moderate fatigue may still be active in chemo intervals. Deficiency signs: pulses, voice, gait. | |
| Cumulative effect of chemo: fatigue last longer, pulses less forceful. | |
| Acu/TCM principle | Invigorate- use draining points not tonify. 30 min. |
| Rx: Li11, Li4, SP9, Liv2, Du20, Kd1 | |
| One day prior to Chemo, 1-2 x per week. | |
| Incorporate exercise, get massage. | |
| post chemo chronic fatigue | Kd jing/Qi def., “lacking a second wind”, constitution state of low energy, cold signs, desire warm. |
| Tonfiying, gentle treatment: big points (ST36, Sp6, Li10), few needles, 30 min. , 1-2 per week | |
| TDP lamp, Qigong, Nutrition. | |
| Heat toxicity- li4, li11, st44, liv2, st36, pc6 | |
| Liver qi stag,: Gb34, Liv3, Li4, St25 | |
| Phelgm obstruction: TB5, ST40, SP9 | |
| Spleen Qi Def: Ren6, Ren12, Sp6, BL20, 21 | |
| Heat Blood def.: HT6, SP6, BL17 | |
| KD Qi Def.: Ren 6, SP6, KD3, Du20 | |
| Hot Flashes | Sudden feeling of warmth, usually intense over face, neck, and chest. Skin may redden like blushing. |
| Profuse sweating can occur and patient can feel chilled. | |
| Pathophysiology | Mechanism not fully understood. Multiple complex hormonal reactions |
| Estrogen, norepinephrine, and serotonin release. | |
| dysfunction of thermoregulatory center caused by changes in estrogen levels. Vasomotor. | |
| causes | Premature menopause, chemotherapy, Oophorectomy. Men: prostate CA on androgen deprivation tx. |
| Systemic antiestrogen TX for hormone-receptor Br Ca. (Tamoxifen) | |
| Hot flash in cancer | 70%. Common, persisting, worse sleep, more fatigue, poor QOL. |
| Tx: estrogen based therapies, but contraindicated in Cancer. | |
| Venlafaxine(75mg), Citalopram (10mg), paroxetine, gabapentin (900mg), pregabalin, clonidine. | |
| RTC: electro-acupuncture was beneficial in treating hot flash. | |
| Decision to use acupuncture | sociodemographic- clinical – cultural |
| attitude- perceived effectiveness of acupuncture | |
| subjective norms- decision support from family and doctors | |
| behavioral control- practical concerns related to using acupuncture. | |
| Preference for natural therapies and symptom appraisal leads to decision to use acupuncture. | |
| Patients claim tey just do not want to take any more pills and choose acupuncture. | |
| Oncology acupuncture: HF | Norepinehprine thought to be primary neurotransmitter responsible for lowering the thermoregulatory set point. |
| Triggers the heat loss mechanism (perspiration, vasodilation) | |
| norepinehprine production and release thought to be inhibited by endorphins | |
| Acupuncture release of endorphins and there inhibit norepinehprine. | |
| Thermoregulatory temperature | |
| dysfunction in hot flashes | 1. core body temperature threshold/baseline changes |
| 2. brain – neurochemical imbalance | |
| 3. peripheral vasculature- changes in vascular reactivity. | |
| Patient experience | QOL, Sleep, Anxiety, Social interactions (we want to know these, if HF affecting this) |
| Assessment | Frequency of HF? |
| Intensity of HF? | |
| Duration of HF? | |
| Time of Day or night? | |
| Night sweats? | |
| Men: Degarelix (Firmagon) GnRH inhibitor. Gonoadotraphin releasing hormone antagonist. Prevents prod of testosterone. | |
| Leuprolide (Lupron Depot) Lutenzing hormone-releasing hormone agonist, prevent prod of testosterone. | |
| TCM patterns | Kidney Yin vacuity |
| Kidney yang vacuity | |
| Dual vacuity of Kidney yin and Yang | |
| Toxins invading channels. | |
| treatment planning | Start: 2x a week followed by weekly. |
| Needle retention 30 min. | |
| 10 treatments in initial course. | |
| points: | L11, Kd3, Kd6, Sp6, Liv2, Liv3, Ren 4, Ren6, Du 20, |
| Erjian: heat clearing auricular apex ear, ear seeds. | |
| E-stim: ST36 and sp6. SP6 and Liv3. (increase the release of beta endorphin activity). 2Hz | |
| Lifestyle: avoid/limit intake | Alcohol, caffeine, nicotine |
| hot and spicy foods, hot beverages, excess sugar. | |
| maintain healthy weight, overweight increases HF | |
| Exercise regularly, in a cool environment, avoid exercise before bed | |
| dressing in layers: patient can remove layers as needed. |
| Provider- Patient communication | Emotional: life perspective changes, fear of recurrence and mortality, hardship in future planning |
| identity shifts, societal and cultural expectations | |
| Physical-psychological: body image adjustments, scars, permanet changes due to surgeries, sexuality/intimacy, | |
| Fertility, reconnecting with body post-treatment. | |
| Pediatric | Parents play a key role in child’s medical care and treatment plan |
| Important to establish and engage in relationship with parents and caregivers. | |
| Appropriate playful interactions are helpful when treating children. | |
| Young adult | Life interrupted during prime self development |
| unique levels of isolation felt through treatment experience | |
| Strong desire to complete life cycle development tasts prior to death, aides in more intense goals for survival | |
| potential to be withdrawn and disengaged with providers, family, friends. | |
| Older adults | potiential for minial caregivers to assist with physical needs and advocacy |
| with more time to establish themselves, difficulty letting go to independence. | |
| Family | Emotionally tied unit. Biological and close friends. |
| Family illness: illness, disability, death are universal experiences in families. | |
| Family concerns should be understood and addressed. | |
| Assessment and management of distrss in families at end of life is vital, family relationships can predict individual distress at the end. | |
| Consider multipe perpectives and narratives. | |
| Partners | Sexual intimacy, fertility concerns, grieving multiple losses as a couple, facing new normal together, future uncertainies. |
| Parents | Child’s health after treatment, anxiety about recuurence and life never being the same. |
| Siblings | Being the healthy one, being the sick one, each feeling guility. |
| Children | will parents be ok? Are they going to leave me? Will they die? Can they give attention? |
| Friends | expect you to return to normal activities, worries you wont relate the same way, |
| feeling differrent than peers, expect you are over cancer. | |
| Patient culture/values/beliefs | Let them tell you who they are, what is important, what they believe |
| Be aware of your own assumptions, biases, how and what they communicate, what medical chart says of prognosis. | |
| Phase 1: initial diagnosis | patient will be overwhelmed, destablized until treatment plan is in place. |
| Clinician role- manage anxiety and fear. | |
| communication strategy: establish rapport, build theraputic alliance. When patient trusts they will reach out. | |
| Phase 2: during treatment | May start to feel physical symptoms and side-effects. |
| Patient feels more focused on goals to complete treatment | |
| Strrategy- do not focus on prognosis, but on treating rthe physical and emotional symptoms. | |
| Phase 3- post treatment | Most patients are excited to not do multiple medical appointments. |
| They want to move beyond the cancer, some still feel emotional impact, anxiety and sadness can settle in. | |
| Some face long-term side-effects. | |
| Strategy- acknowledge their feelings, normalize their fears, introduce new rapport and ways to keep relationship going. | |
| Try to to dis-regard their needs because they are cancer free. | |
| Phase 4: recurrence | Emotion can hit harder, more fragility in mood. Physical symptoms increase. |
| Balancing of patients wishes to talk about fears, death, and remaining hopeful surface. | |
| Strategy: do not be afraid to talk about fears, remain curious how they perceive recurrence, let them guide the talk. | |
| Phase 5: end of life | Some patients struggle to accept prognosis |
| Some can acknowledge their death and wish to engage in life reviews, legacy discussion. | |
| Help them stay relaxed as possible to alleviate suffering physically. | |
| Strategy: be present, emphaty, be silent, hold the space for these patients. | |
| Stay in the “here and now” focus on the moments. Gain better self-awareness of your own death and anxiety, | |
| how that impacts your communication with patients end of life. | |
| Difficult patient or caregiver | Acknowledge their frustration, contain the situation as best as possible. |
| Wrap up treatment if behavior escalates. | |
| Don’t hesitate to speak to the unacceptable nature of any aggression towards you. | |
| Seek supervisory assistance when necessary. | |
| Try to remember that their emotions are often a displacement of worry for themselves or loved ones. | |
| Family / friends during treatment | Look at medical chart, ask patient if they want to share medical chart if family/friends asks quesitons, otherwise no. |
| Inform medical team if you cannot respond. | |
| As a provider you play an important role in alievating both physical and emotional symptoms. | |
| Talking about Integrative medicine | patients will ask about many types of therapies they hear about on internet. |
| Patients want to explore all options for a disease with poor prognosis | |
| Usually dissatisfaction with current available treatment. | |
| Patient empowerment. | |
| when talking with patients | maintain open mind and empathetic attitude. Listen. Look for deeper issues. |
| figure out what the patient really needs. Formulate a plan that is evidence based and tailored to their needs and preference. | |
| Use the opportunity for a comprehensive counseling on health. | |
| Counseling | Open convo by acknowledge their interest in integrative medicine |
| State your role of working with physician | |
| Provide opportunity for patient to voice any questions or concerns | |
| Explore underlying reasons for questions and concerns.analyze the questions and concerns. | |
| Expaln why some therapies without scientific backing may be harmful | |
| Introduce concept of integrative medicine for well-being, body, mind, spirit, | |
| Offer lifestyle assessment and recommend changes. | |
| Discuss therapies appropriate to patients concerns, situations and needs. | |
| Summarize key points of the conversation. | |
| Confirm patients understanding and that all questions have been answered. | |
| Document the encounter for paitents primary physician. | |
| Arrange follow-up visits to monitor adverse reactions and response to treatment. | |
| Adjust treatment plan as required. | |
| Complementary therapies | A: Safe and helpful |
| B: safe but not enough data if helpful | |
| C: Useful but with risk (herbals can be here due to side effect or interaction with other drugs) | |
| D: Harmful and no benefit. | |
| Mind-body therapies that are safe: | Meditation, hypnosis, guided imagery, biofeedback, |
| breathing, muscle relaxation, yoga, qigong, tai chi | |
| Benefits | Reduce common emotional and psychological problems |
| Stress reduction may have influence on the pathophysiology of disease thus improve outcome | |
| Helps caregivers to deal with the stress of caring for a chronically ill patient and build a nurturing family environment. | |
| Improve the well-being of the physician, making them more emotionally balanced and effective at work, | |
| more job satisfaction and better care for patients.(for caregivers/physicians who do mind-body therapies) | |
| Mindfulness vs TM (Mantra) meta study | Comparison of meditation programs with nonspecific active controls (efficacy). |
| psychological stress and well being. | Anxiety- Mindfulness had a moderate improvement, while TM had low to no effect. |
| Depression- Mindfulness had a moderate improvement, while TM was insufficient. | |
| Stress/Distress: Mindfulness had low improvement, while TM had low to no effect. | |
| Negative effect- Mindfulness had low for improvement, while TM was insufficient. | |
| Positive effect: Mindfulness was insufficient, while TM was insufficient. | |
| Quality of Life: Mindfulness was low improvement. | |
| Attention: Mindfulness was insufficient. | |
| Sleep: Mindfulness was insufficient | |
| Substance use: TM was insufficient | |
| Pain: Mindfulness had a moderate improvement, while TM was low to no effect. | |
| Weight: TM low to no effect. | |
| Overall the study did favor meditation over the control. 47 trials with 3515 participants, | |
| JAMA Intern Med. 2014 Mar, 174 (3): 357-68. | |
| Yoga meta-analysis | Favors Yoga for Anxiety, stress, depression, QoL, Distress, Fatigue. |
| Massage therapy | Swedish, Reflexology, Lymphatic drainage, Myofacial release, shiatsu |
| Tui-na, Reiki, Ayurvedic massage | |
| Best effects were mood and pain. | |
| Acupuncture for cancer | Found to be effective for pain, nausea, vomiting |
| Useful for: Hot flashes, insomnia, dry mouth, anxiety | |
| Exploratory: GI dysfunction, Lymphedema, Fatigue, Neuropathy. | |
| Herbs and dietary supplements | Natural products are rich source of theraputic agents that are biologically active.(some drugs come from plant materials) |
| Supplements are perceived as safe, not true in some cases, may have side effects of interact with other drugs. | |
| Some products are hyped up with unsubstantied claims and even fraudulent. | |
| Phytoestrogens | red clover, kudzu, alpha-alpha, wild yam, resveratrol, grape seeds, fo-ti, dongquai, chaste berry, licorice |
| Soy. Avoid soy isoflavone supplements. Food: low serving of tofu, soy milk, soy nuts, miso, soy protein, bean spouts. | |
| Supplements | Read the fine print. Dose may be small |
| Many have small amounts of active ingrediant. | |
| Integrative medicne approaches | Patient centered: patients responsibility and ability in taking in an active part in their health care. |
| Physician’s responsibility in inspiring and empowering patient to do so. | |
| Proactive: Emphasis on prevention | |
| Focus on fostering the body’s resilience in order to resist diseases and recover from illness. | |
| Holistic: recognize the importance of body-mind-spirit interaction in well being. | |
| Incorporate non-conventional therapies that have a favorable risk/benefit ratio. | |
| Improve mental resilience | Attitude: stay positive, deflect negativity, be gently, be able to let go. |
| Self-Improvement: remain true to yourself, joyfulness, meanings and priorities, spiritual growth. | |
| Grading recommendation | A, B, C, D, H (against the service moderate or high it can harm), I (insufficeient evidence, need more study). |
| finally: | Be open and empathetic, evidence-based discussions of complementary therapies. |
| help patients needs be understood. Lead them to reduced symptoms and better QoL. | |
| help them avoid hearmful therapies, enhance trust and rapport, strengthen the physician-patient relationship, | |
| improves the overall quality of patient’s care. | |
| Safety in clinical practice | patients have complicated medical histories. Disease and conventional treatment cause a wide range of effects. |
| anxiety and depression are common psychological comorbidities. | |
| Referrals to acupuncture in the inpatient hospital setting by MD/NP/PA for inpatients. | |
| Chart review: Physician notes- best source. | |
| Diagnostic tests: Radiology (CT scans, MRI, X-ray), Pathology, Recent blood tests. | |
| Oncology treatment history: chemotherapy, Radiation, surgery, additional medications. | |
| acupuncture history: | Prior experineces, response, sensitivity to needles, phobia, size, manipulation, |
| realistic expectation with acupuncture, prognosis and goals. | |
| Precautions and contraindications | Thrombocytopenia- bleed risk. Platelet counts: normal is 160-400k/mcl. Cancer: 20 to 50 or <20 needle shallow or hold off. |
| neutropenia- infection risk. WBC normal is 4.0 to 11 k/mcl. Low is 1.5 to 8.8 k. below 0.5 hold off. | |
| mental status issues: erratic behavior | |
| Fever/active infections | |
| Severe weeping edema | |
| Lymphedema | |
| Avoid recent surgical stie area | |
| Site of tumor or metastates | |
| area of recent XRT | |
| Thrombosis (DVT) | |
| Cardia arrhythmias, patients on pacemaker (no estim) | |
| Medical devices | IV lines, PICC lines, NG tube, Medi-port, Hepatic artery pump |
| EKG, BP, O2 monitoring, Ventilator, Catheter, Drain. | |
| Surgical concerns | Patients can be heavily medicated following surgery |
| Tissue expanders, ostomies, sutures, drains, surgical site- bandages, avoid local area | |
| Amputation- phantom limb pain, skin grafts. | |
| Metastasis | Brain- cognitive changes or confusion |
| Spine- avoid aggressive needling | |
| Pelvis- avoid deep needling and strong stim | |
| Skin- avoid skin lesions, decreased integrity, malignancy. | |
| Emergent situations | Onset of SOB, increase HT rate by 20 bpm, Alert RN/MD. |
| Document event, do not be afraid to ask for help. | |
| Universal precautions | Treat everyone as if they could have HIV, HBV or other blood born pathogens. |
| Hand washing, gloves, masks, gowns when appropriate. | |
| Hand: before touching patient, before antiseptic procedure, after body fluid exposure, | |
| after touching aptient, after touching patient surroundings. | |
| 62% ethyl alcohol before and after acupuncture. | |
| Soap and water- hands are visibly soiled, dirty, contaminated. Before and after activities with risk of blood or fluids. | |
| Patients isoloated due to drug resistant infections. After bathroom, before eating. | |
| Ppe: gloves, gowns, masks, respirators. Remove before exiting the room. | |
| have good SOAP notes: intervention , service provided, clinical notes, patient visits, correspondence to professionals. | |
| brachytherapy | Internal radiotherapy |
| EMR/EHR records are best. Electronic charting. | |
| Herbs and Drug interactions (HDI) | 30% of cancer survivors use herbs |
| 63% of cancer survivors with chronic illnesses use more that two supplements | |
| The average amarican uses 12 Rx drugs per year | |
| ADRs resulted in >100,000 deaths per year | |
| 2004 the study of herbal effects on metabolism and other toxicity. | |
| Grapefruit and St. John’s wort can interact with drugs. | |
| Mechanisms can be traced back to co-evolution of pants and humans. | |
| PubMed only has about 1000 articles on herb interactions. Needs more clinical trials and studies. | |
| top herbs | St. John’s Wort, Ginkgo, Kava Kava, Digitalis, Willow, asian ginseng, astragalus, licorice, saw palmetto, garlic |
| top drugs interacted | Warfarin, Insulin, aspirin, digoxin, ticlopidine, theophilline, cyclosporin, heparin, spironolactone, tamoxifen |
| FDA study in 2006: | 75k calls to poison control: 275 were oabout dietary supplements, 112 signs of toxicity, 6 HDI, 3 ICU, 1 death (caffeine and yohimbe) |
| Herbs and Drug interactions (HDI) | species, part of plant used, quality control, dosage, duration of use |
| Patients | Genetics, age, gender, disease state, liver and renal function, diet |
| Drugs | Dosage, route of administration, pharmacokinetics |
| Pharmacokinetic | absorptoion- distribution- metabolism- elimination |
| Pharmacodynamic | Herbs affect the pharmacologic properties of other herbs and drugs. |
| Absorption- | increases GI motility- decreaed absorption, pH- Ionization weak acid vs weak base, effects on enteric coated drugs. |
| Solubility and physical compatibility: fat can increase lipophilic drug absorption, minerals and tannins from plants | |
| can bind with drugs and decrease their absorption. | |
| Blood flow- increase intestinal blood flow increase absorption. | |
| Distribution | protein binding- drugs transported by binding to albumin. Only the unbound drugs are active. |
| Herbs exibit higher affinity to proteins and displace drugs into the free (active) form resulting in: | |
| Increased toxicity and altered drug assay. | |
| metabolism | Oxidation and reduction, congugation with glucuronate or acetate- water soluble metabolites, |
| facilitates excretion of kidney urine and liver bile. | |
| inducers- increase enzyme or transporter activities. | |
| substrates- substances metabolized by microsomal enzymes or affected by transporters. | |
| inhibitors- decrease enzyme or transporter activities. | |
| Herbs can make treatment infeffective or it can Increase adverse events. | |
| Juices with CYP3A4 inhibitory effects | Pomegrante, Pomelo, cranberry, seville orange, lemon |
| Interactions cancer treatment | blood thinning herbs vs anticoagulants (warfrin: avoid garlic, ginkgo, ginseng, dong quai, st john wort, feverfew) |
| Antioxidants vs chemo drugs (chemo drugs: avoid grape seed extract and pine bark extract) | |
| Phytoestrogens vs hormones (avoid ginseng, soy, dong quai, red clover) | |
| immunostimulants vs immunosuppressants. (avoid astragalus/huang qi for patient on immunosuppresants) | |
| Manage interactions | Monitor high risk patients closely |
| Adjust dosing intervals | |
| Change route of administration | |
| Change or discontinue one or both agents | |
| Enhance communication between healthcare providers and patients. | |
| Obtain relevant information. | |
| www.aboutherbs.com | |
| Integrative approach to Cancer prevention | reduction of caner mortality via the reduction of cancer incidence. |
| Avoid carcinogens, smoking cessation, | |
| Change lifestyle and diet to modify cancer-causing factors | |
| Take medication to reduce risk of cancer (Chemoprevention), tamoxifen can prevent breast cancer in high risk women. | |
| screen for early detection to remove precancerous lesions (colonoscopy to remove polyps) | |
| Avoid radiation- use sunscreen, avoid unnecessary X-rays and CT scans. | |
| Treat or prevent infection- vaccine or Rx. HPV (cervical cancer), HBV, HCV (liver cancer), | |
| Epstein-barr virus (Burkitt lymphoma) H.pylori (gastric cancer) | |
| Obesity | Postmenopausal breast cancer |
| Cancer of esphagus, pancreas, colorectum, endometrium and kidney. | |
| Other: Coronary heart disease, diabetes type II, cancers, hypertension, dyslipidema, stroke | |
| Liver and GB disease, sleep apnea, osteoarthritis, gynecological issues. | |
| Reduce calories by 500-1000 per day. | |
| Increase physical activity, 30 minutes daily, moderate intensity. | |
| Behavior therapy- self monitor, stress management, social support, integrative therapies. | |
| Foods- red meat, processed meats, alcoholic drinks, sugar. | |
| More dietary fiber, more fruits, non-starchy vegetables, vitamin D | |
| Physical activity | decreaes inflammation, decreae insulin resistance, reduce adipose tissue. |
| increase cancer survival | |
| 8 things to help prevention | Body fatness: Be as lean as possible. |
| Physical activity- limit sedentary habits, 30 minutes vigorous physical activity. | |
| Foods: avoid high calorie foods, sugary drinks, fast food, energy drinks. | |
| More pant foods- increae servings to 5, unprocessed grains, legumes, limit starchy foods. | |
| Reduce red meat, pork, lamb, salted foods, smoked foods. | |
| Limit alcohol drinks. | |
| Aim to meet nutritional needs through food and less with supplementation. | |
| www.mskcc.org/aboutherbs |
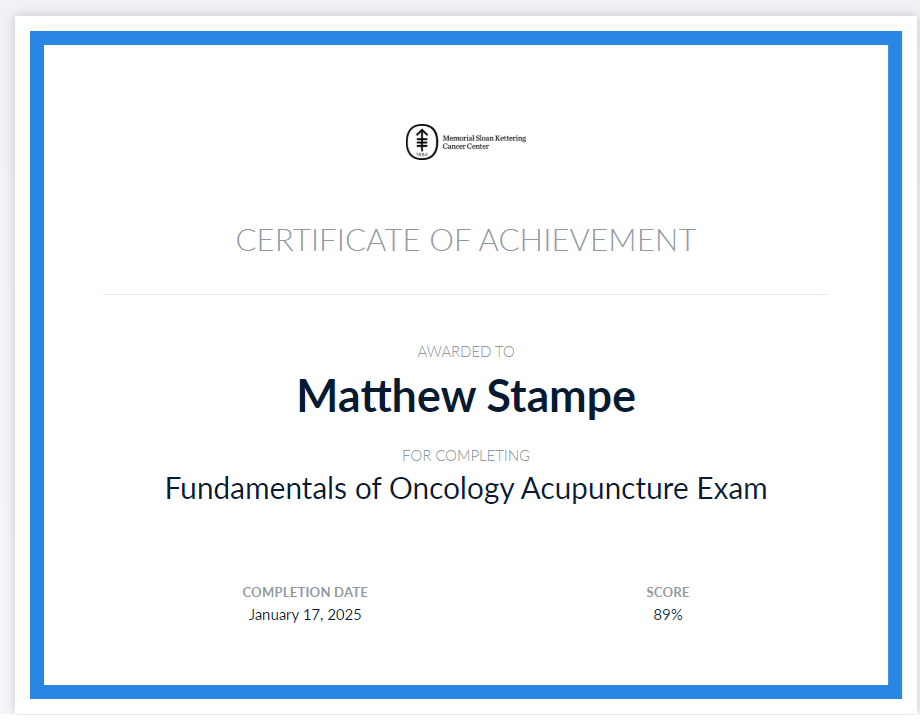
| Survivorship | Cancer survivors are seeking the best path to change their lifestyle and improve their overall healthy, |
| as well as decrease their risk of cancer recurrence. | |
| Survivorship definition: having no signs of cancer after finishing treatment. | |
| Living with, through nad beyond cancer. | |
| Begins at diagnosis, through treatment to the rest of person’s life. | |
| Transition | Period of time leading up to completion of therapy through initial phase afterward. |
| Individuals living with advanced or metastatic disease are often overlooked as candidates for rehabilitation. | |
| Rehabilitation and survivorship support includes physical therapists, occupational therapists, and speech-language pathologists. | |
| Survivor statistics | 16.9 million people with a history of cancer living in the US on Jan. 1, 2022. |
| Cancer survivors in the US , expected to reach 22.1 million by 2030. | |
| Survival often comes with physical, psychosocial and financial burdens. | |
| Cancer Rehabilitation | Many Cancer networks (NCCN, ACS ACCC, etc.) now identify rehabilitation as a crucial if not mandatory component of cancer care. |
| Many centers do not have organized programs for cancer rehab. | |
| TCM/Acupuncture/herbalist | can be a component of usual care to help patients suffering from late effects caused by cancer and its treatments. |
| We can assess health status and subtle changes in our patients in frequent time points. | |
| We can provide whole system individualized care that can address multiple complaints simultaneously. | |
| We tend to have regular contact with our patients so are able to provide ongoing evaluations of potential changes or | |
| signs of recurrence. | |
| Fear of cancer recurrence (FCR) | Lifestyle factors can be related to FCR. High FCR in patients who were smokers, low FCR in patients who had healthy habits. |
| Physical activity, “5-A-Day” (servings of fruit and veggies), quit smoking. | |
| Chemotherapy/drugs side effects | chemo brain, heart conditions, thyroid problems, lung damage, infertility, Osteoporosis, hearing loss |
| Cataracts, secondary cancers, peripheral neuropathy, impaired immunity | |
| Radiation therapy side effects | Hyper/hypo thyroid, hearing loss, vision problems, dry mouth, brain or thyroid cancer, osteoporosis. |
| Radiation to the chest | Lung damage, breathing difficulties, heart damage, osteosarcoma, breast cancer, thyroid cancer, hyper/hypo thyroid |
| Immune therapy- still new and learning | Car T-cell therapy, B-cell aplasia and resulting hypogammaglobulinemia, as well as prolonged cytopenia’s and infection risks. |
| ICI- immune checkpoint inhibitors: nivolumab, pembrolizumab, atezolizumab, ipilimumab. | |
| Assessing the patient | |
| factors to consider | Type of Cancer, cancer treatment, location of tumor, common sites for metastasis, age and health at diagnosis, TCM constitution |
| Collect patients experience of symptoms prior to cancer diagnosis and treatment, during cancer treatment, and present. | |
| No two patients are the same, it will be common their medical presentations will be hard to understand. | |
| Cancer Recurrence | Conventional medicine does not have a tool to predict recurrence in a particular patient. |
| Patients will be put on a schedule for follow-up. Annual change for 5 years post treatment. | |
| It is important for us to keep a close watch on any changes in the patient’s presentation. | |
| Some cancers have a higher rate of recurrence than others. | |
| Each cancer has different monitoring. | |
| Conventional medicine does not emphasize lifestyle counseling. | |
| Metastasis | Know where cancer tends to spread. |
| Be mindful of early symptoms of cancer in distant areas, be first to recognize this. | |
| Include inquiry and assessment of these sites in survivor patients. | |
| Red Flags | Loss appetite, weight loss/changes, night sweats, fatigue, and pain. |
| Symptoms of metastasis | Brain: headaches, seizures, nausea, vomiting, weakness, confusion, visual disturbances |
| Bone: local pain | |
| Liver: rt. Side abdominal pain, jaundice, fatigue, weight loss, nausea. | |
| Understanding of survivors of Cancer. | |
| Breast Cancer | Most common non-skin cancer, second leading cause of death, survival remains steady since 2000. |
| side effects: GI complaints, lymphedema, cardiac toxicity, reproductive dysfunction, neuropathy, skin changes, skin changes | |
| radiation fibrosis, fatigue, hot flashes. | |
| 5 year survival is 89%, cancer can move to lung, liver, bones, brain. | |
| Recur around surrounding area lymph, look for swelling under the arm, collarbone, neck. Changes in skin, thickening or redness | |
| Cognitive dysfunction, bone loss, neuropathy, endocrine disruptions, infertility, sexual health issues, body image concerns. | |
| risk factors | Breast traversed by liver channel and stomach channel through nipple |
| Chong and ren dysfunction | |
| Chronic constraint | |
| External pathogen like wind-cold invasion bind with blood for form lumps | |
| Fire toxins invade organs to cause inflammatory breast cancer | |
| Damp invasion | |
| Over work, overwhelmed, unresolved grief, unexpressed emotions | |
| Cold foods damaging spleen. | |
| hot flashes | Hormonal treatment, chemotherapy induced ovarian failure, ovarian suppression therapy, surgical menopause. |
| Frequency, severity, triggers, time of day, symptom journal. | |
| sweat pattern, temperature before and after. | |
| DX | Qi stagnation, blood stagnation, damp accumulation, Yin deficiency, shao yang disharmony, Qi level heat. |
| Prognosis | Usually by treatment 4, goal minimizes symptoms. |
| Colorectal Cancer | Increased screening has led to early detection. |
| decrease in QOL | |
| effects: fatigue, sleep difficulty, fear of recurrence, anxiety, depression, negative body image, sensory neuropathy, | |
| GI problems, urinary incontinence, sexual dysfunction. | |
| 1.4 million survivors, 90% survival with early detection | |
| tends to met in liver and lung or abdominal cavity | |
| sx of local recurrence: frequent stools, thinner stools, feeling incomplete bowel movement, | |
| blood in stool, loss of appetite, abdominal pain or fullness. | |
| side effects: bowel or bladder dysfunction, sexual dysfunction, peripheral neuropathy, mental health, risk of pelvic fracture, cardiotoxicity. | |
| Leukemia | acute lymphocytic (ALL) |
| chronic lymphocytic (CLL) | |
| Acute Myelogenous (AML) | |
| Chronic Myelogenous (CML) | |
| Mortality down 1% each year since 2000 to 2010 | |
| late effects: fatigue, risk of another cancer, early cardiac disease. | |
| Blood Cancers | majority of leukemia relapses occur up to 2 years after treatment. |
| look for bruising, swollen lymph nodes, bone or joint pain, recurrent infections. | |
| Lymphoma | Hodgkins- mortality decreased by 70% since 1975. Incidents the same |
| Non-Hodgkins: mortality decreased; incidence decreased | |
| Late effects: increase risk of other cancers for up to 20 years, early cardiac disease | |
| Lung disfunctions, xerostomia, hypothyroidism, infertility | |
| Lung Cancer | Primary cause of cancer related death, mortality declining since 2001, |
| late effects: Lung dysfunction, pain, neuropathy, fatigue. | |
| Tends to met to brain, bone, liver | |
| Recurrence symptoms: coughing, blood in sputum, shortness of breath, wheezing, pain in chest | |
| Fatigue, pneumonia, CIPN, depression. | |
| risk factors: EPF invade lungs and impair diffusing and downward bearing, toxic heat leading to yin vacuity | |
| exuberant phlegm-damp, emotional depression, chronic spleen vacuity. | |
| Prostate Cancer | most common non-skin cancer, second leading cause of death in men |
| Incidence rose dramatically when began to use PSA test | |
| 90’s mortality has declined. | |
| Late effects: erectile dysfunction, urinary and bowel trouble, infertility | |
| 5-year survival is 95% | |
| Tends to spread to liver, lungs, bones (hip, spine, pelvis), and lymph | |
| 30% can relapse after 5 years. PSA increases after treatment. | |
| Urinary, sexual or bowel dysfunction. | |
| ADT can cause increased risk for obesity and diabetes as well as cardiovascular disease | |
| Bone density loss. | |
| Gynecological cancer | Ovarian- tends to met to bone, liver and brain. |
| 70% of ovarian cancers recur (50% within 3 years). | |
| Abdominal swelling or pain. Urinary changes if it compresses the bladder. | |
| Uterine- tends to met to the lungs, bones, brain, vagina, pelvic organs | |
| 88% recurrences in first 3 years | |
| More than 50% are symptomatic. | |
| Childhood cancer survivors | Late effects of childhood cancers: death if primary cancer returns, second malignancy, Heart and lung damage from treatment. |
| Need to know patients’ history since many late effects develop years later. | |
| Comon late effects: Organ, tissue and body dysfunction, growth and development delay | |
| Depression, anxiety, challenges with learning and memory, social adjustments, risks of secondary cancers. | |
| Late effect symptom management | Cardiac Toxicities: chemo drugs Trastuzumab, Doxorubicin, Daunorubicin (Cerubidine) |
| Eprirubicin (Ellence), Cyclophosphamide (Neosar). | |
| high blood pressure: Bevacizumab (avastin), sorafenib (Nexavar), Sunitinib (Sutent). | |
| Chemo brain- affects anyone who has had chemotherapy, becoming a late-effect. Difficult thinking, concentration, memory. | |
| Fatigue: most common reported, can go on for years, 25% more common in women. | |
| Hot flashes: caused by medically or surgically induced menopause | |
| Lymphedema: common after lymph node removal in breast surgery, high risk of infection on affected limb. | |
| Xerostomia: radiation effect, difficult to treat, start treatment as soon as possible. | |
| Sexual dysfunction: erectile dysfunction, vaginal dryness, pain with intercourse, body issues, hormonal changes. | |
| Neuropathy- begins during treatment and becomes chronic, further away from treatment can make recovery difficult. | |
| Fear/anxiety: recurrence can be severe, “watch and wait” up to 5 years or more, Shame. | |
| insomnia: Often begins during treatment and continues in survivorship, related to treatment or anxiety. | |
| infertility: patients can bank egg and sperm before treatment, loss of fertility can be devastating. | |
| pain: chronic pain is common, 40% reported, screen for pain every visit, recurrent diseases, second malignancy, | |
| important to consider using a validated pain measure in survivors. | |
| Pain Red flags: new onset should be evaluated, assess patients’ opioid use, consider referral to MD for screening. |
| Hospital Based Practice | Columbia university Dept. of Pediatrics |
| Michelle Bombacie NCCAOM, Lac, LMT. Kenna Bouvet, Lac, CPT | |
| overview of policies, procedures, practice guidelines in hospital based integrative medicine center | |
| Intgrate acupuncture and communicate collaborative approach with a convential cancer setting | |
| Needle education and research | |
| Implementation of this model through case presentations. | |
| Risks scenerios and still being effective. | |
| JCAHO: Joint commission on Accreditation of Healthcare Organization | |
| WHS: Workplace Health and Safety. Infection prevention, , HIPPA, OSHA training. Contact isolation example. PPE | |
| NIH. National Center for comlimentary and Integrative health. | |
| NIH: Acupuncture: Mind body category (acupuncture, qigong, Massage, yoga) EBM, Whole systems. (ayervedic,osteopathy, TCM, chiro, PT) | |
| Credentialing: state license, Malpractice insurance, NCCAOM, Course work on patient population. | |
| Education: doctorat, Masters, etc., years of experience. | |
| Standard Operating procedures (SOP) | new patient recruitment, consenting patients |
| (nutritionist, yoga instructor, etc. | Ititianl tratment planning, Ongoing tratment planning |
| Acupuncture specific protocols | |
| Patient assessment for acupuncture | |
| Patient encounter requirements | |
| Patient tracking and charting | |
| Daily logs | |
| Wellnes program | |
| Supportive care guidelines | Recommendations and strength and quality of evidence |
| best practices | |
| Hiqh quality: confident in the estimate of effect | |
| Moderate quality: further reseasrch as important impact of confidence of effect | |
| Low Quality: further research very likely to have a imprtant impact on confidence of effect. | |
| Very low quality: estimate of effects are uncertain | |
| Chemo Ind. Nausea Vomit (CINV) | acupuncture strongly recommended. Hypnosis, systemic desensitization, or relaxation techniques (MBSR) |
| Fatigue | acupuncture strongly recommended. Physical activity, systemic desensitization, or relaxation techniques (MBSR) |
| EMR | collects data. Platelet assessment, signs/symptoms, TCM diagnosis |
| 5 phase diagnosis, treatment plan, advesre events, total needles in/out, retention time, technique, needle type. | |
| Points used, extra, ears, unilateral, bilateral. | |
| Scales (pre and post acupuncture) 1-10 | distress like Anxiety (1-10) |
| Nausea and vmiting | |
| Pain (1-10) | |
| Fatigue | |
| Neuropathy | |
| Other | |
| RASCAL | Research compliance and administration . IRB institution review board |
| Allows to create protocols, appendicies, COI’s (conflict disclosure) create HIPPA and consent forms. | |
| Thrombocytopenia | acupuncture was fine considering low platelents, no infections or excess bleeding reported |
| Neutropenia | low WBC count, there was no infections were reported from acupuncture |
| Integration and translation of acupuncture | |
| Integrative Therapies program | nutritioninst, acupuncturist, physicla therapist, occupational therapist, research corrdination. |
| acupuncture, acupressure, aromatherapy, exercise and movement, massage, mnd-body medicine, nutiritional counseling | |
| CIHT (complementary integrative health therapies) | Natural products |
| Deep breathing and breath work | |
| Acupuncture, Acupressure | |
| Aromotherapy acupoint therapy (Jeffery Yuan method) | |
| Yoga, Tai Chi, Qigong, | |
| Chiropractice and Osteopathic services | |
| Meditation | |
| Massage, canial sacral, Reiki, reflexology, Tui-na | |
| Heat, kinesio tape | |
| Special Diets | |
| Homeopathy | |
| Progressive relaxation | |
| Guided imagery | |
| Typical day in clinic | Patient check in, triaged and labs, visit with NP or oncologist, if patient makes counts then chmo is ordered |
| RN assess patietn, visit with psychologist, visit with nutritonist, visit with intgerative therapist, | |
| If patient does not meet counts they only see CCQ or ITP | |
| Acupuncture to patient | Acupuncture stimulates acupoints on meridians on surface of body. Neurotransmitters modulate pain chemicals, |
| acupuncture regulation of activity of pain sensation, changes brains processing of informaiton and neocortical, limbic, and brainstem levels. | |
| it alters purinergic signaling, treatments are individualized on constitutional and circumstantial (root and branch). | |
| Assessment approach to treatment | Root treatment: support earth (kids weak ST/SP), fear, fright, (kidneys), Fu zheng Pei Ben (upright Qi, prevent cancer growth) principle. |
| Acute treatment: symptom managemtn ans patient is experiencing it | |
| Prevention: understanding treatment protocol and working to prevent chemotherapy | |
| Chronic: persistent symptomatology | |
| Zang fu: yin/yang organ pair involved or influenced | |
| Meridians: pathway trajectory: what organ system to they enter and/or encase | |
| Substances: What substances are involved in diagnosis of treatment protocol | |
| 5 element: depending on age, observation of being. | |
| TCM Oncology | Blood level Xue: Leukemias. TCM: heart governs, Liver stores and regulates, spleen contains. |
| Marrow: Leukemias, Brain and CNS tumors. TCM: Kidney, extraordinary organ, Brain. | |
| Phlegm: Solid tumor, Lymphomas. TCM: Spleen, blood stasis, Kidney, Liver. | |
| Jin shen pediatrics (5 phase observation) | water: 1-3 monthsn, 6-7 years, 13-14 years |
| wood: 3 months to 1 year, 8-9 years, 15-16 years | |
| Fire: 1-2 years, 9-10 years, 16-17 years | |
| Earth: 2-3 years, 11-12 years, 17-18 years | |
| Metal: 4-5 years, 12-13 years, 19-20 years. | |
| water: flexible, slow, observer, delayed milestone, fearful, imaginative, withdras easily | |
| Wood: action, very active, quick temper, restless, assertive, thrills, frustrated | |
| Fire: bright, active, entertainer, seeks stimulation, magnetic quality, overexcited, dramatic | |
| Metal: detailed, organzied, sensitive, routine, aesthetic sense, hyper focuses, rigidity | |
| Assessment: approach to Tx | Emotion |
| Physiology | |
| Structure | |
| Side effect prevention: | pain, anxiety, constipation, headache, URI, UTI, immune weakness, appetite, CIPN, mucositis, scars, sleep difficulty, trauma response |
| radiation: anxiety, burns, skin sensitivity, dryness, brain fog | |
| surgery- amputation, prosthesis, posterior fossa syndrome, tumor resection, ventrical peritoneal shunt. Anxiety, pain, scarring. | |
| Procedure: lumbar puncture, Intra oral chemotherapy, port placement, scans, transfusions. Anxiety and pain. | |
| medical team check-in (Red flags/Cautions) | ANC < 0.5 k/mcl |
| Platelets <20k | |
| blood clots | |
| unstable vital signs | |
| tumor break through/ metastatic site | |
| anatomical changes and scar tissue associated with surgery | |
| change in medical diagnosis | |
| C-diff | |
| Needle type | Pyonix, or smallest seirin needle for kids. |
